Medical Education
Session: Medical Education 2
537 - PSP in Practice – A Pediatrics Curriculum for Learning about Health Care Disparities and Social Determinants Through Clinical Experience
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 537
Publication Number: 537.551
Publication Number: 537.551

Meredith Volle, MD, MPH (she/her/hers)
Assistant Professor of Clinical Pediatrics
Southern Illinois University School of Medicine
Springfield, Illinois, United States
Presenting Author(s)
Background: Pediatricians know how to care for individual patients, but to effect change for pediatric populations they must also understand systems factors. It is known that disparities in health care (HCD) and health outcomes are rooted in social and structural determinants of health (SDH), yet residents and faculty may fail to recognize evidence of this in clinical encounters. Few faculty have formal education in SDH and HCD, which can reinforce the hidden curriculum, perpetuate discrimination, and lead to dissatisfaction among trainees who want to understand how to apply these topics in practice. The pediatrics residency program at our institution reviewed ACGME survey results and found that our residents reported a perceived need for more education on SDH and HCD, despite examples in all subspecialties and explicit teaching in multiple rotations. Our program worked with the population science and policy education team to address this among all learners in clinical settings.
Objective: To integrate HCD and SDH into the curriculum; to increase recognition and reinforce HCD/SDH in clinical settings; to help residents/faculty teach these topics to medical students.
Design/Methods: Residents and faculty received specific examples of SDH and HCD in pediatrics, including systemic barriers and policies that impact pediatric health outcomes, and pathways to teach these concepts. Curriculum was also delivered during each clerkship, reinforcing the role of residents as learners and teachers. Residents also explored these topics in depth through the Advocacy/Palliative Care rotation. Surveys of students and residents were conducted twice a year to evaluate knowledge, confidence, and teaching of SDH and HCD. Data was collected using RedCap. ACGME survey reports were also reviewed.
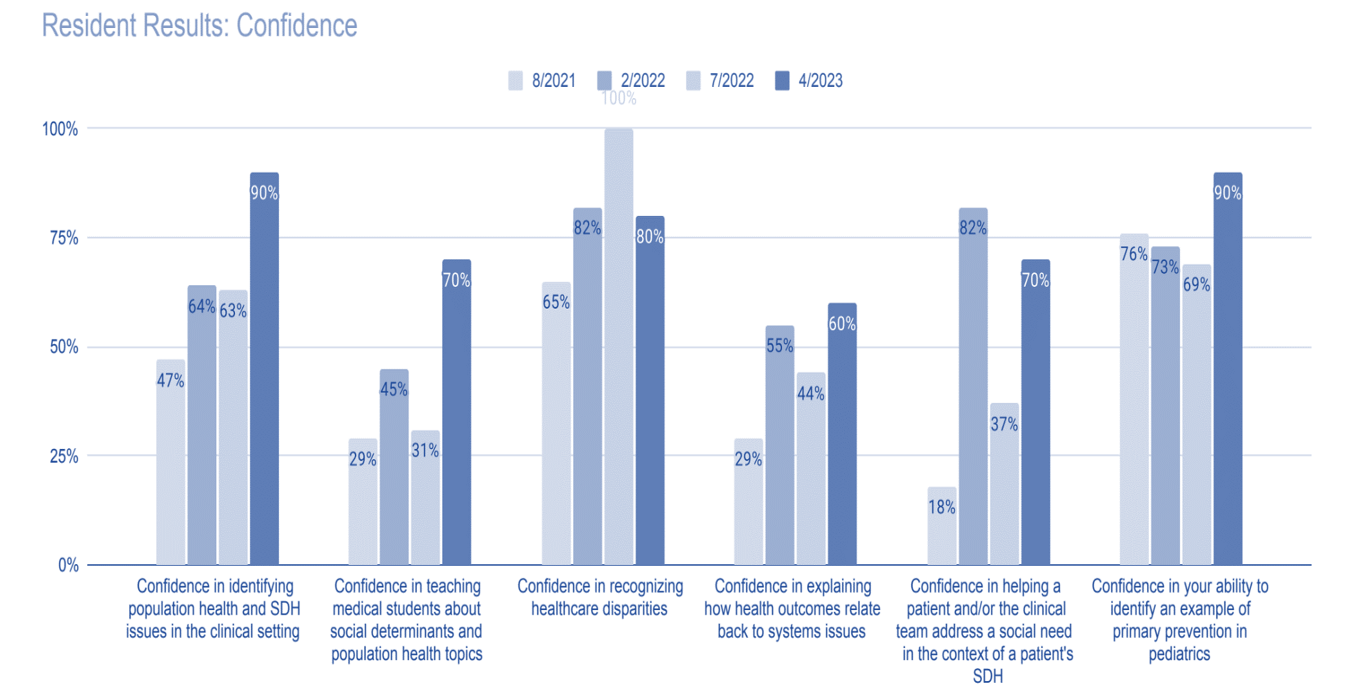
Results: In 2020-2021, the ACGME survey reported 68% program compliance for “taught about HCD,” compared to 84% in all pediatrics programs. After these changes program compliance rose to 90% (compared to 83% all) in 2021-2022. Residents’ self-reported confidence on SDH in clinical settings also increased 43%, and HCD rose 15%.
Conclusion(s): Pediatric trainees who understand these concepts are better prepared to practice medicine that is effective and equitable. Through small adaptations in one year our program was able to assist learners make clinical correlations to SDH and HCD. Limitations: voluntary surveys and variable participation; confidence is a subjective, self-reported measure. Future work will examine sustainability of curricular changes and ways to measure effectiveness of resident education on SDH and HCD on health outcomes.