Hospital Medicine
Session: Hospital Medicine 4
143 - Quality Improvement Initiative for Improving Interdisciplinary Communication by Utilizing EPIC Chat Feature in the Pediatric Inpatient Setting at an Urban Teaching Hospital
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 143
Publication Number: 143.1135
Publication Number: 143.1135

Arthi Ramu, MBBS (she/her/hers)
Resident Physician
SUNY Downstate Health Sciences University
Brooklyn, New York, United States
Presenting Author(s)
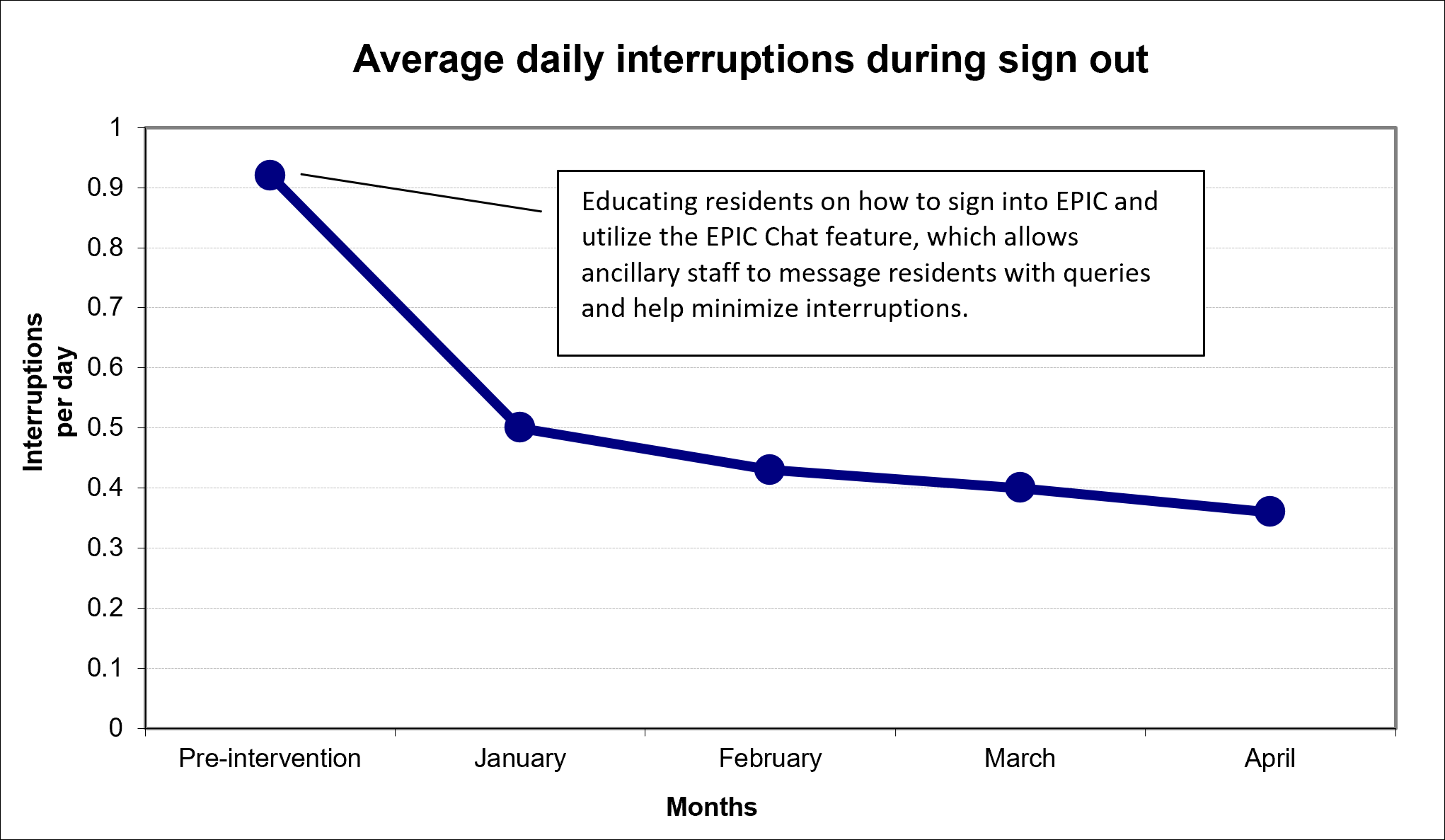
Background: Structured and efficient communication methods among care providers in an inpatient setting is required to optimize patient care, minimize communication failures, and prevent medical errors. In our inpatient unit, the resident workroom is in close proximity to the nursing station, resulting in frequent direct communication between the healthcare team members. While this may provide an immediate and convenient mode of communication, it often leads to interruptions during provider handoffs and transitions of care. These communication failures increase the risk of preventable medical errors and adverse patient outcomes. Our quality improvement (QI) project aims to standardize the use of EPIC Chat on our electronic medical record to improve communication amongst various providers.
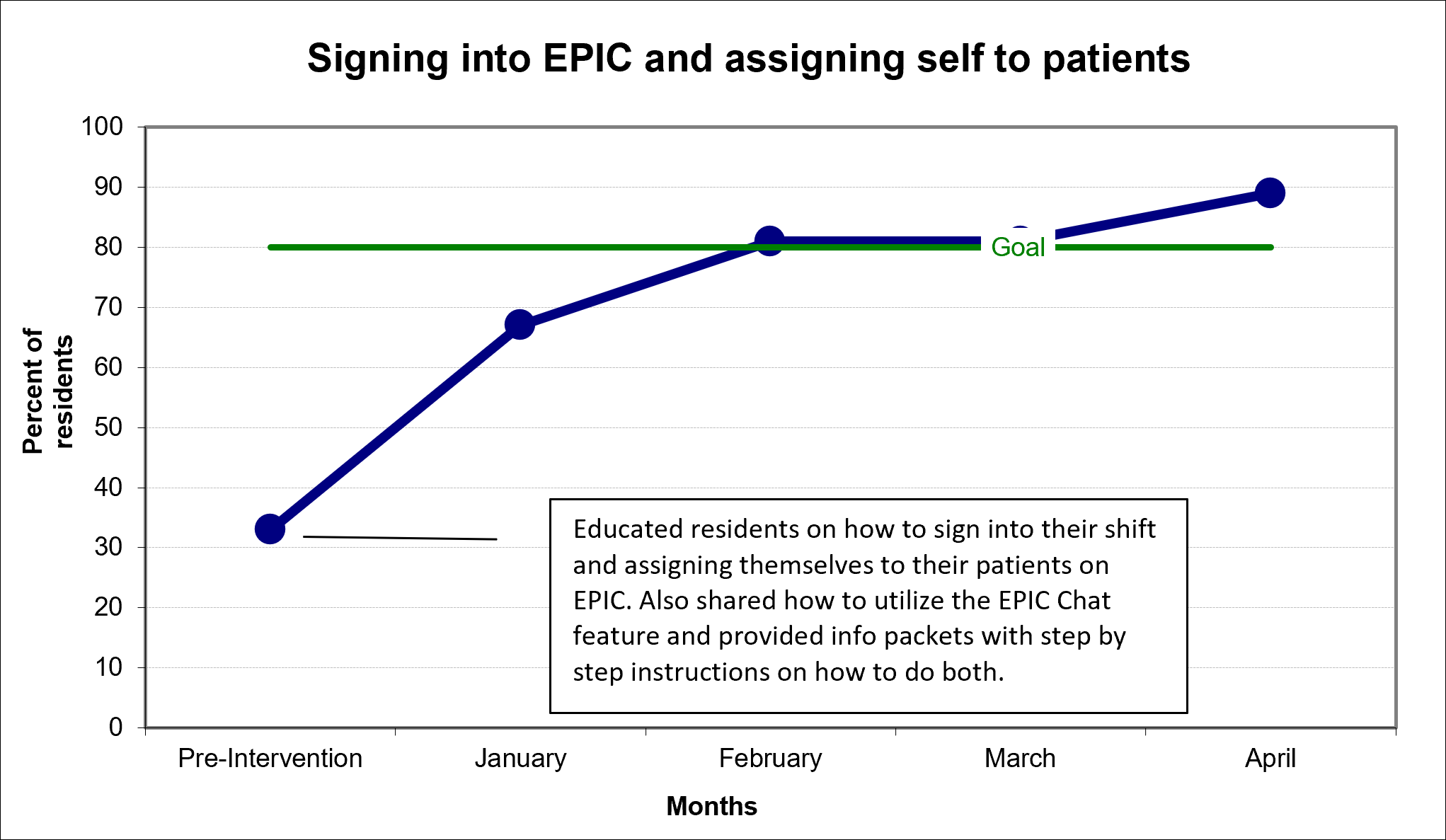
Objective: Our QI project’s primary aim is to improve rates of residents and nurses use of EPIC Chat in the pediatric inpatient setting to 80% within a four-month period. Our secondary aim is to minimize interruption during handoff and improve interprofessional communication.
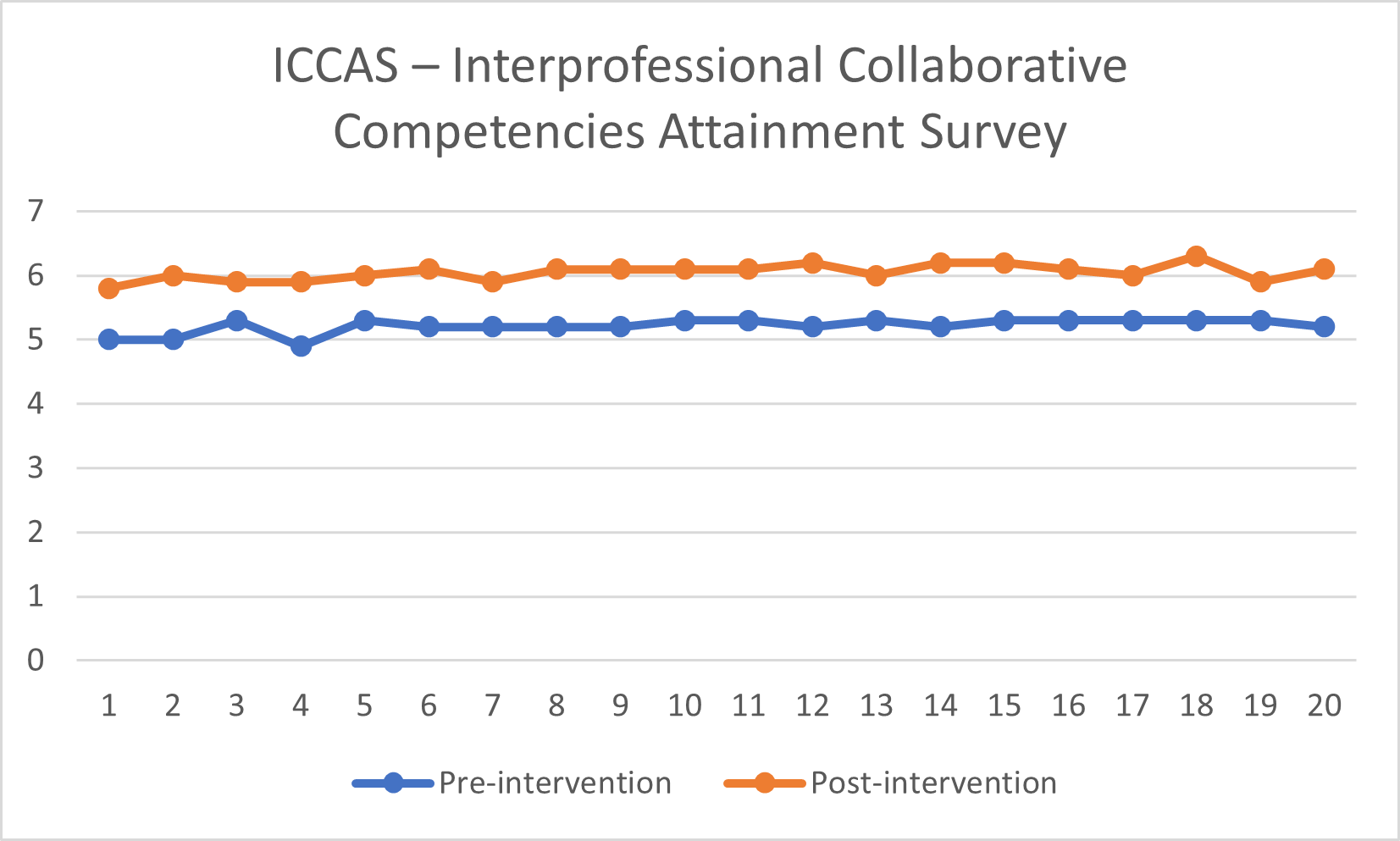
Design/Methods: The QI Model for Improvement was used to guide our interventions. Three types of baseline data were obtained: number of residents signing into their patients daily, number of interruptions during sign-out and completion of a validated Interprofessional Collaborative Competencies Attainment Survey (ICCAS). This survey was administered to the residents and nurses pre- and post-intervention to assess behaviors associated with patient-centered, team-based, collaborative care. Monthly educational sessions were held at the start of each inpatient block to orient all residents and nurses on the use of various features on EPIC to facilitate communication. Simplified information packets were also provided including the information reviewed during the sessions.
Results: During the 4-month period of our QI project, rates of residents signing into EPIC and their patients each morning improved from 33% to 89% (Fig.1). The rates of interruptions during sign-out decreased from 0.92/day to 0.36/day (Fig.2). On reviewing the ICCAS data, the residents and nurses overall felt an improvement in their level of communication and ability to provide patient-centered collaborative care (Fig.3).
Conclusion(s): We surpassed our target, increasing rates of residents signing into and utilizing EPIC Chat to reach the goal of 80% as early as 2 months post-intervention. This project showed us that by utilizing the simple yet effective feature on EPIC to help facilitate communication and minimize interruptions, we can help optimize healthcare delivery.