Neonatology
Session: Neonatal Infectious Diseases/Immunology 3
621 - Corticosteroids enhance endothelial restitution through alterations in TGF-b signaling
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 621
Publication Number: 621.558
Publication Number: 621.558
- TB
Timothy J. Boly, DO (he/him/his)
Instructor of Pediatrics
University of Iowa Stead Family Children's Hospital
Iowa City, Iowa, United States
Presenting Author(s)
Background: Following inflammatory stimulation, the endothelial barrier becomes permeable to allow for movement of leukocytes from the vasculature to sites of infection or injury. In neonatal capillary leak syndrome (CLS), following extreme inflammatory injury, the barrier breaks down excessively allowing serum contents to leak into the interstitium, worsening the clinical illness of the infant. Endothelial cell proliferation and migration are regulated through the TGF-b pathway, but through two co-receptors. ALK1 promotes cell proliferation and migration, while ALK5 inhibits these processes. Corticosteroids are used in the treatment of CLS for their anti-inflammatory properties, but their effect on endothelial healing has not been investigated.
Objective: The purpose of this study was to evaluate the effect of corticosteroid on endothelial restitution and to determine their effect on the expression of TGF-b co-receptors, ALK1 and ALK5.
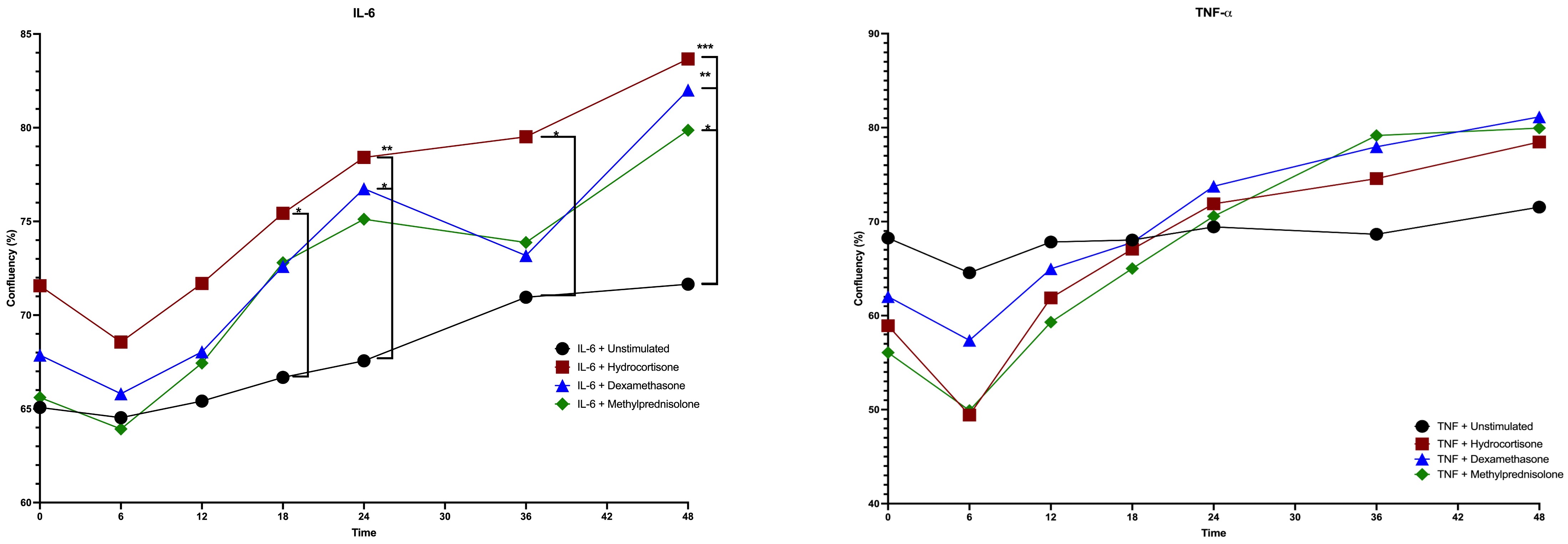
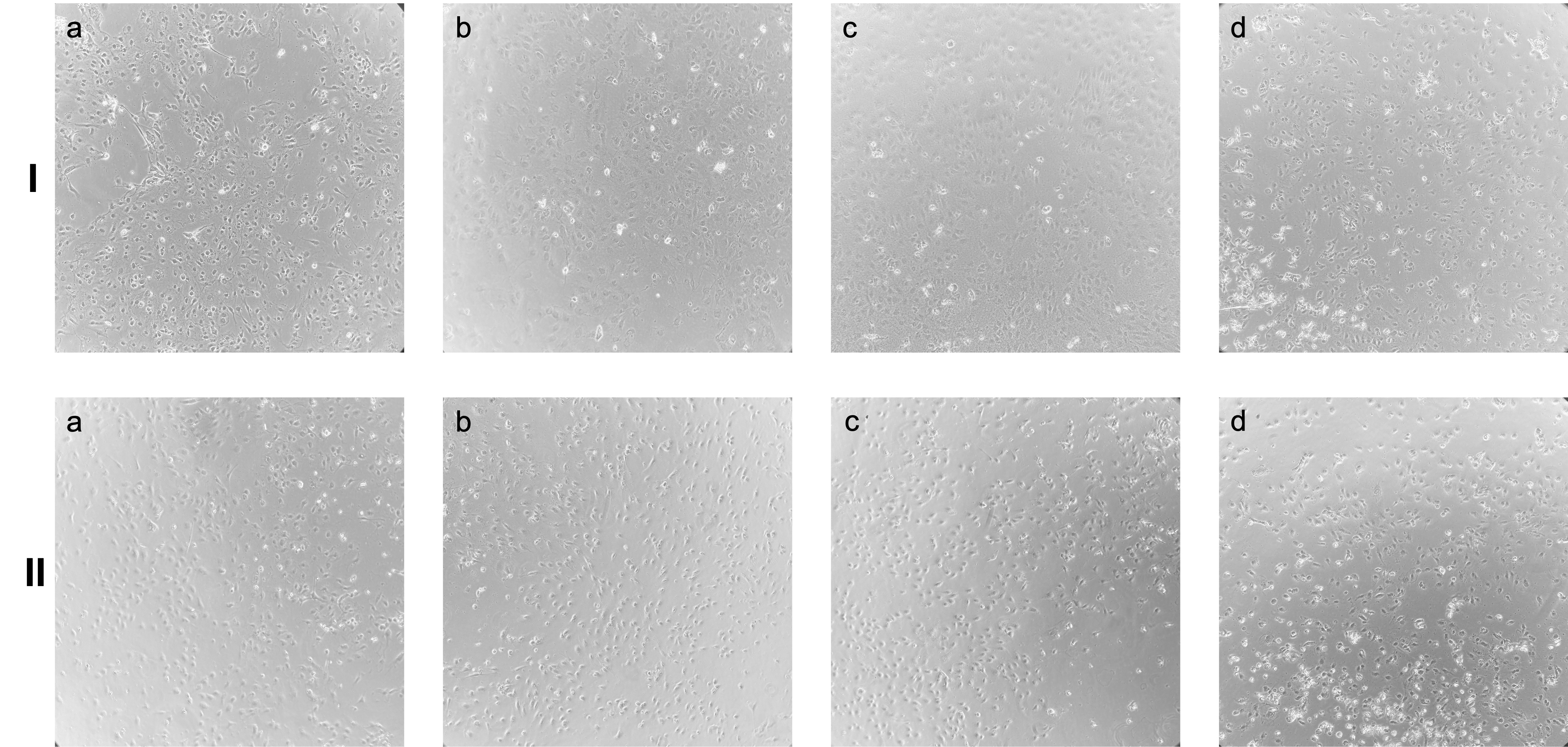
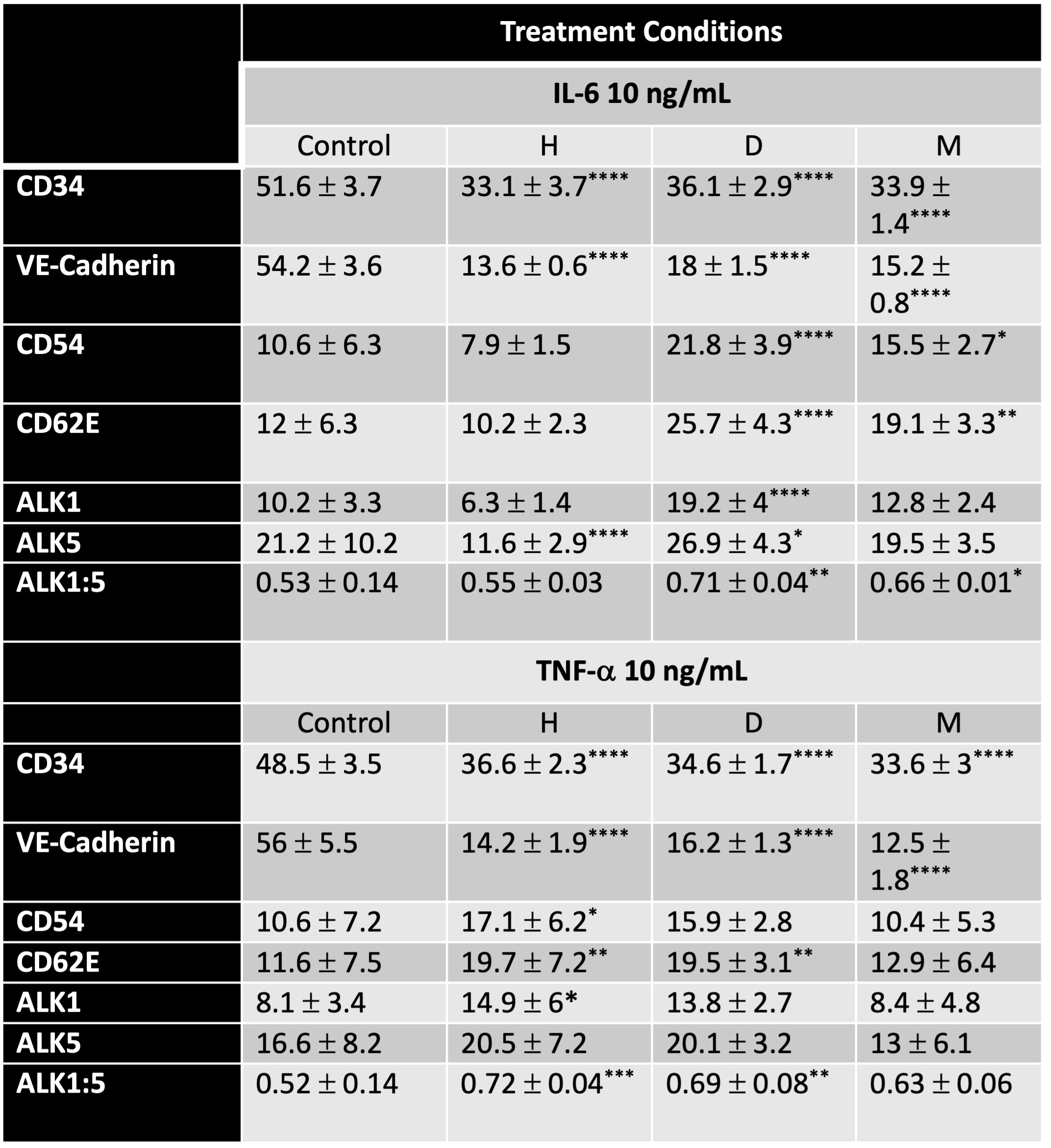
Design/Methods: Human umbilical vein endothelial cells (HUVECs) were maintained in culture. For the healing assays, HUVECs were grown to confluence and then starved for 24 hours. The cells were then inflamed with IL-6 10 ng/mL or TNF-a 10 ng/mL for 6 hours. HUVECs were treated with hydrocortisone 25 ug/mL, dexamethasone 2.5 ug/mL, or methylprednisolone 12.5 ug/mL for 48 hours. Untreated cells were used as a control. Interval microscopy was performed, and ImageJ software was used to measure confluency after treatment. Analysis of variance (ANOVA) was used to determine differences. For flow cytometry, the same above conditions were repeated, however HUVECs were only treated for 24 hours. Flow cytometry was used to evaluate CD34, VE-Cadherin, CD54, CD62E, ALK1, and ALK5. ANOVA was used to determine differences in cell markers between the different conditions.
Results: 48 hours following treatment, HUVECs inflamed with IL-6 were significantly more confluent with all steroid therapies as compared to control (n=9, Figure 1A, 2A). No significant differences were seen in those treated after TNF injury (n=9, Figure 1B, 2B). Flow cytometry demonstrated steroid treatment following inflammation significantly increases the ALK1:ALK5 ratio as compared to control (n=8, Table 1).
Conclusion(s): In addition to their anti-inflammatory properties, corticosteroids increase the surface expression of the ALK1 co-receptor on HUVECs, leading to restoration of the endothelial barrier through TGF-b signaling. This mechanism provides additional evidence for the benefits of corticosteroids in neonatal CLS. Future work examining the interplay of TGF-b and corticosteroids is underway.