Medical Education
Session: Medical Education 3
543 - Building a Scholarly Community: Assessment of a Novel Professional Development Program for Pediatrics Junior Faculty
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 543
Publication Number: 543.568
Publication Number: 543.568

Laura Chappell-Campbell, MD (she/her/hers)
Clinical Assistant Professor, Pediatric Hospitalist
Stanford University School of Medicine
Palo Alto, California, United States
Presenting Author(s)
Background: There is an important need for junior faculty professional development. In January 2021, our institution launched a novel faculty development program for pediatric junior faculty. The Peer Scholarship Communities (PSC) aimed to support scholarship and career development via creation of four communities focused on specific domains of interest (Clinical Research, Global Health, Medical Education, and Quality Improvement). Each community consisted of 2-3 senior mentors and 5-12 junior faculty participants who met regularly as small groups for two years. Biannual retreats brought participants from all communities together for works in progress presentations and workshops.
Objective: To assess the impact of the PSC program on faculty engagement, mentorship, and scholarly productivity among program participants.
Design/Methods: In January 2021, we conducted a pre-survey of faculty members in the first cohort of participants entering the PSC program. A follow up post-survey of the same population was conducted in May 2023. The de-identified, IRB-approved surveys included questions on engagement, scholarly productivity, mentorship, and professional development needs. The post-survey also explored participants’ perceptions on the benefits and shortcomings of the program. We used descriptive statistics for the quantitative data and grounded theory and content analysis for the open-ended questions.
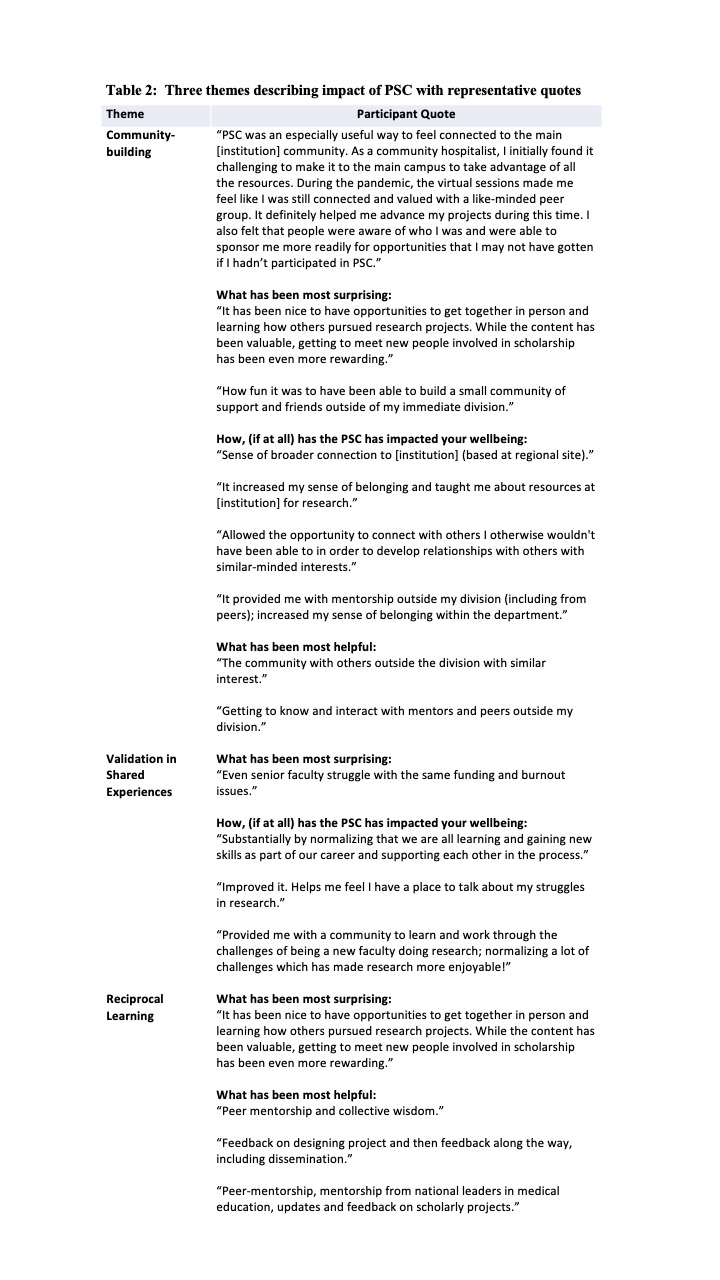
Results: Of 34 faculty in the cohort, 28 completed the pre-survey and 19 completed the post-survey. 17/19 (89%) participants would recommend the PSCs to others. Participants described 3 major benefits: 1) Community-building: Participants emphasized developing strong relationships with peers having similar scholarly interests, particularly across academic divisions, and fostering a sense of belonging. 2) Validation in Shared Experiences: Participants appreciated discussion of shared struggles and learning from the challenges faced even by senior mentors. 3) Reciprocal Learning: Participants benefitted from workshopping peers’ work and receiving feedback from peers and senior mentors. Challenges included the amount of time required, conflicts with clinical work, insufficient scholarly productivity, and difficulty determining meaningful topics for discussion.
Conclusion(s): Interdivisional faculty development programs centered on domains of professional interest can support scholarship while fostering community-building and collaboration, contribute to participants’ sense of well-being, and provide valuable opportunities for shared learning.
.jpg)