Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 4
19 - Baseline Capacity and Early Quality Improvement Results for Primary Care Sites Participating in a Pilot Collaborative to Improve Pediatric Overweight/Obesity Treatment Visits
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 19
Publication Number: 19.2780
Publication Number: 19.2780

Janice Liebhart, MS (she/her/hers)
Evaluation Manager
American Academy of Pediatrics
Itasca, Illinois, United States
Presenting Author(s)
Background: The 2023 pediatric obesity guideline (CPG) recommends that primary care teams (PCTs) comprehensively evaluate patients ages 2-18 with overweight (OW) or obesity (OB) for comorbidities and offer them multicomponent, family-based, intensive health behavior & lifestyle treatment, ideally >=26 contact hours over 3-12 months. Because PCTs often lack local resources to help provide treatment, there is an urgent need to help them build capacity. A 33-week team-based, virtual quality improvement (QI) collaborative, based on the Model for Improvement, was launched in April 2023 to support PCTs in offering OW/OB treatment visits. The pilot integrates new CPG-focused resources, including a detailed capacity assessment tool, a comprehensive Key Driver Diagram, training modules and a change package of clinical & patient-facing tools.
Objective: To describe baseline capacity and early clinical measure results for the pilot
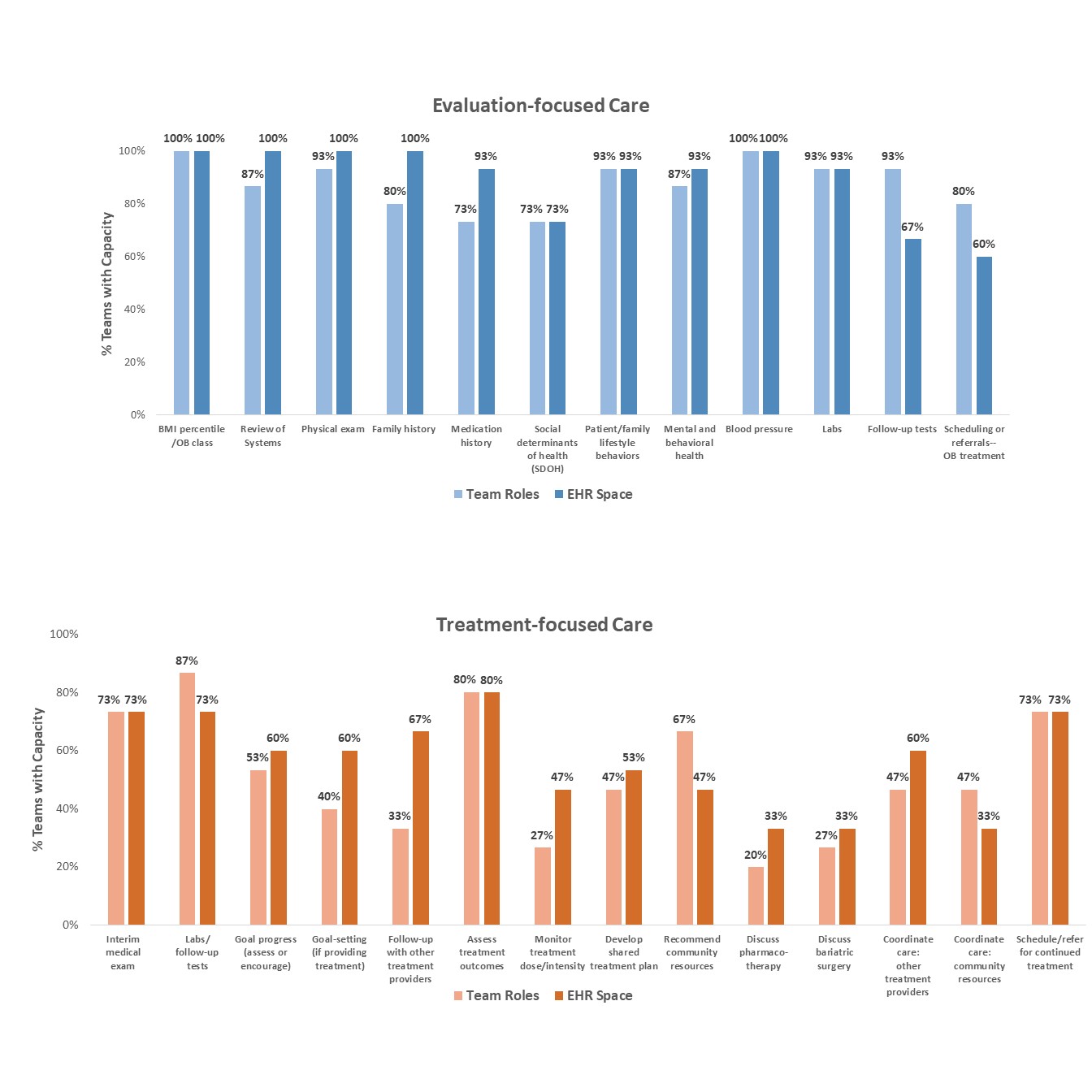
Design/Methods: PCTs at 15 diverse practice sites completed the baseline capacity assessment. Questions included the % staff (in quintiles) trained in 6 relevant topics (e.g., CPG, OB stigma). PCTs also reported whether (Y/N) staff roles and electronic health record (EHR) space existed for 12 aspects of care for evaluation (e.g., BMI, labs) and 14 aspects of treatment (e.g., assessing goals; discussing adjuncts), as well as the implementation stage (4 ordered levels) of 15 key systems to support care. Teams repeat the assessment at the end of the collaborative and 4 months later. PCTs submit 3 cycles of clinical data during the collaborative, plus 1 monitoring cycle 4 months later. Data are based on 15 randomly selected treatment visits and used to calculate 7 evaluation- and 8 treatment-focused measures. Analyses are descriptive. Capacity questions with >2 response categories are dichotomized with the lowest 2 categories labeled “low.”
Results: Half or more of PCTs reported low staff training levels for all topics. Most PCTs had roles in place for all aspects of evaluation but lacked roles for 8 of 14 aspects of treatment (Fig.1). EHR space often, but not always, followed staff roles. Most PCTs reported high implementation levels for only 3 key systems: identifying patients, scheduling visits, & billing (Fig. 2). Available aggregate clinical measures (cycles 1-2) suggest that PCTs are making modest progress in improving CPG-related care (Fig.3).
Conclusion(s): Use of a new capacity assessment may help PCTs pinpoint gaps and strategies for implementing and sustaining evidence-based OW/OB treatment visits. Remaining assessments and data cycles will help gauge the value of pilot participation.
.jpg)
.jpg)
