General Pediatrics
Session: General Pediatrics 1
229 - Impact of an Embedded Phlebotomist on Lead Toxicity Diagnosis
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 229
Publication Number: 229.577
Publication Number: 229.577
Yilu Dong, PhD
Assistant Professor
Medical College of Wisconsin
Wauwatosa, Wisconsin, United States
Presenting Author(s)
Background: Lead poisoning is a significant problem in Milwaukee. While 2.5% of children nationally have elevated blood lead levels (BLLs) (≥ 3.5 μg/dL), the percentage is 6.6% in Wisconsin, and 15% in Milwaukee city. Diagnosing elevated BLLs requires a multi-step process including a screening survey, initial capillary point of care test (POCT) and a confirmatory venous test. Interventions to decrease BLL are not initiated until venous tests demonstrate elevated BLLs; interval monitoring is then scheduled. While POCT is available in all primary care clinics, venous testing is only available through centralized labs. Prior to our study, only 28% of elevated POCT BLLs were confirmed.
Objective: Our objective is to assess the impact of an embedded phlebotomist on 1) child conformance rate to confirmatory and interval monitoring venous testing (within 4 weeks from the last elevated results), and 2) time to confirmatory venous testing at the intervention site and a nearby site.
Design/Methods: A prospective study of children with elevated POCT BLLs was undertaken at four clinic sites. The intervention site had an embedded phlebotomist starting 01/01/2023; the nearby site referred to the intervention site (in addition to continuous access to the centralized labs as usual care), and two other (control) sites continued following the usual care. The impacts on conformance rates were analyzed using an advanced difference-in-differences (DiD) with staggered adoption design; time to confirmatory testing was analyzed using a survival analysis.
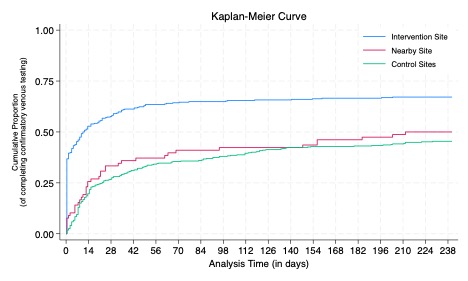
Results: 826 patients with elevated POCT BLL across the four clinics were included (Table 1). The DiD estimates showed the embedded phlebotomist increased conformance rate to confirmatory venous testing by 31.6% (95%CI: 25.7%, 37.5%) at the intervention site, by 15.6% (95%CI: 5.6%, 25.6%) at the nearby site, resulting in an additional 124 children with elevated BLL being confirmed with venous samples. For the interval monitoring testing, conformance rate increased by 25.6% (95%CI: 13.4%, 37.9%) at the intervention site, with no change at the nearby site. The Kaplan-Meier curves showed the cumulative proportion of patients that have completed confirmatory venous testing against time once they tested POCT high at each site (Figure 1).
Conclusion(s): An embedded phlebotomist was effective in increasing patient’s conformance rate to confirmatory and interval monitoring venous testing at the placement site. It marginally benefited patients to the nearby site on confirmatory testing, with no effect on the interval monitoring testing.
.jpg)