Medical Education
Session: Medical Education 9
504 - Improving Resident Leadership Skills During Pediatric Resuscitations Utilizing the CALM Instrument
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 504
Publication Number: 504.2771
Publication Number: 504.2771

Cynthia M. Carter, DO (she/her/hers)
Pediatric Emergency Medicine Fellow
The University of New Mexico
Albuquerque, New Mexico, United States
Presenting Author(s)
Background: Effective leadership is essential during resuscitations and can prevent serious morbidity and mortality. Pediatric residency training rarely includes a structured teaching curriculum of leadership skills. Furthermore, tools to assess leadership skills are often difficult to implement. The CALM (Concise Assessment of Leader Management) instrument is a validated tool that easily and reliably gives constructive feedback to the leaders of pediatric simulated resuscitations but has yet to be applied in a pediatric resident curriculum.
Objective: To determine the utility of the CALM instrument in improving leadership competency and comfort during simulated pediatric resuscitations.
Design/Methods: Twenty-five residents participated as leaders in two simulated resuscitations, separated by one month. Attending physicians were used as raters and used the CALM instrument to assess each resuscitation leadership performance. The CALM assessment has 17 individual measurements which are summed to create a CALM score, a proxy for leadership competence. Day 1: Residents filled out a pre-survey measuring comfort, then participated in 6 resuscitation simulations. Each study participant acted as a team leader during one of those simulations. Team leaders were given brief verbal feedback by raters after the resuscitation. Day 2: The same simulations were used, but residents led a different simulation than on Day 1. Prior to the start of each simulation, the team leaders reviewed their previously filled out CALM assessment with the rater. After this review, the simulations were conducted in the same manner as day 1. Finally, participants filled out a duplicate comfort post-survey. Wilcoxon rank sum tests were used to compare Day 1 and Day 2 CALM and comfort scores.
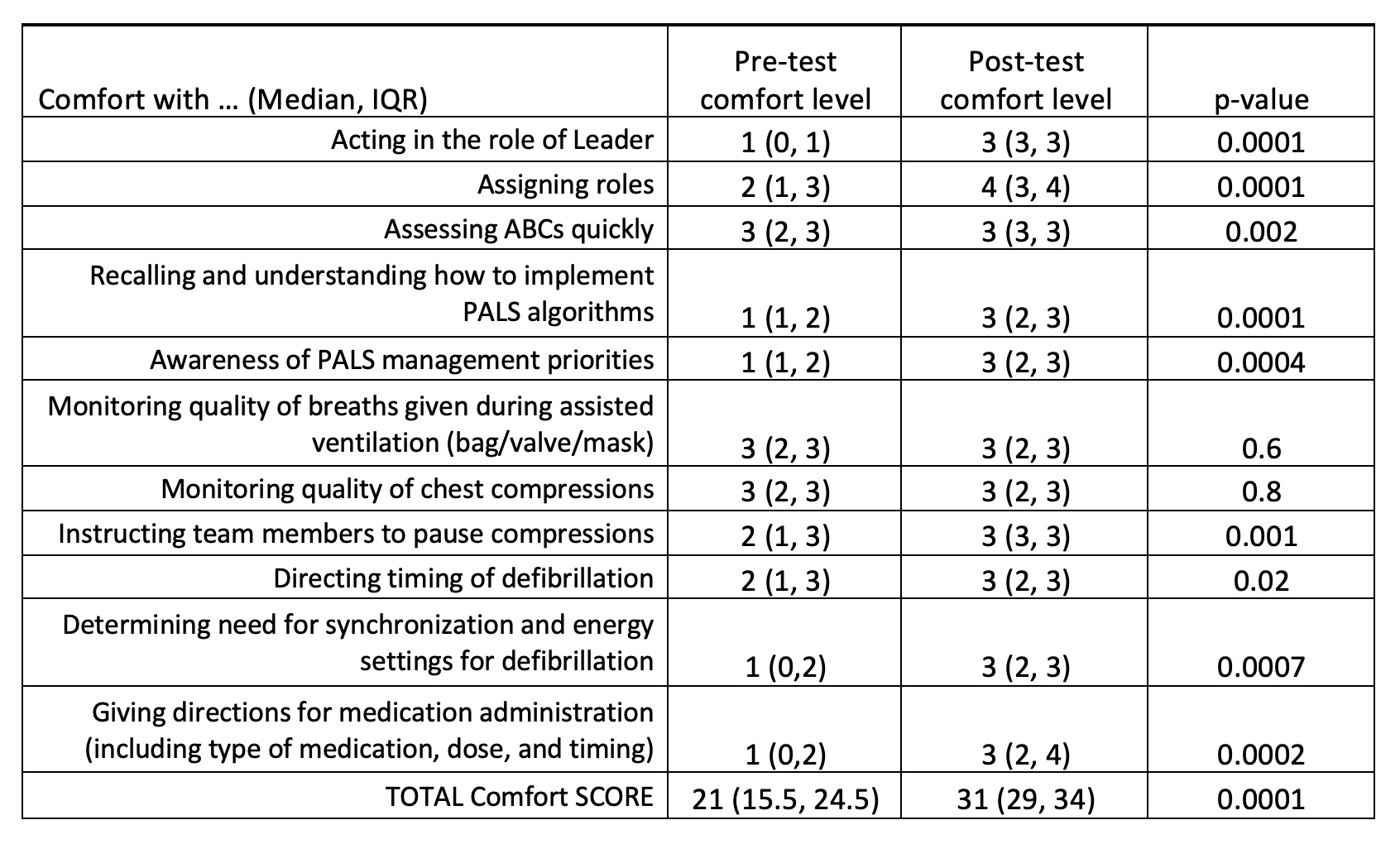
Results: CALM scores increased significantly for the total group of 25 participants (p < 0.0001), as well as for each PGY subgroup: PGY1 (p < 0.005), PGY2 (p < 0.03), and PGY3 (p < 0.02; Table 1). Changes in every individual leadership measurement were significant (Table 2). Total comfort score also increased significantly (p < 0.0001), as did 9 of the 11 individual comfort elements (Table 3).
Conclusion(s): This study demonstrated improvements in leadership competence and comfort in pediatric simulated resuscitation scenarios after assessment and feedback using the CALM instrument.
.jpg)
.jpg)
