Nephrology
Session: Nephrology 4
19 - Collaborative Decision-Making in Youth with Chronic Kidney Disease
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 19
Publication Number: 19.2251
Publication Number: 19.2251

Hyeyoung Ryu, MS (she/her/hers)
PhD Candidate
University of Washington
Seattle, Washington, United States
Presenting Author(s)
Background: Missed opportunities for youth with chronic kidney disease (CKD) to develop and practice decision-making skills in a safe and mentored setting can contribute to poor health-related decisions and self-management. Collaborative decision-making (CDM)—an approach where clinicians, patients, and other key stakeholders (e.g., caregivers) contribute their individual expertise to work together and make well-informed, value-based decisions—has been shown to foster health literacy and improve adherence, clinical outcomes, and quality of life.
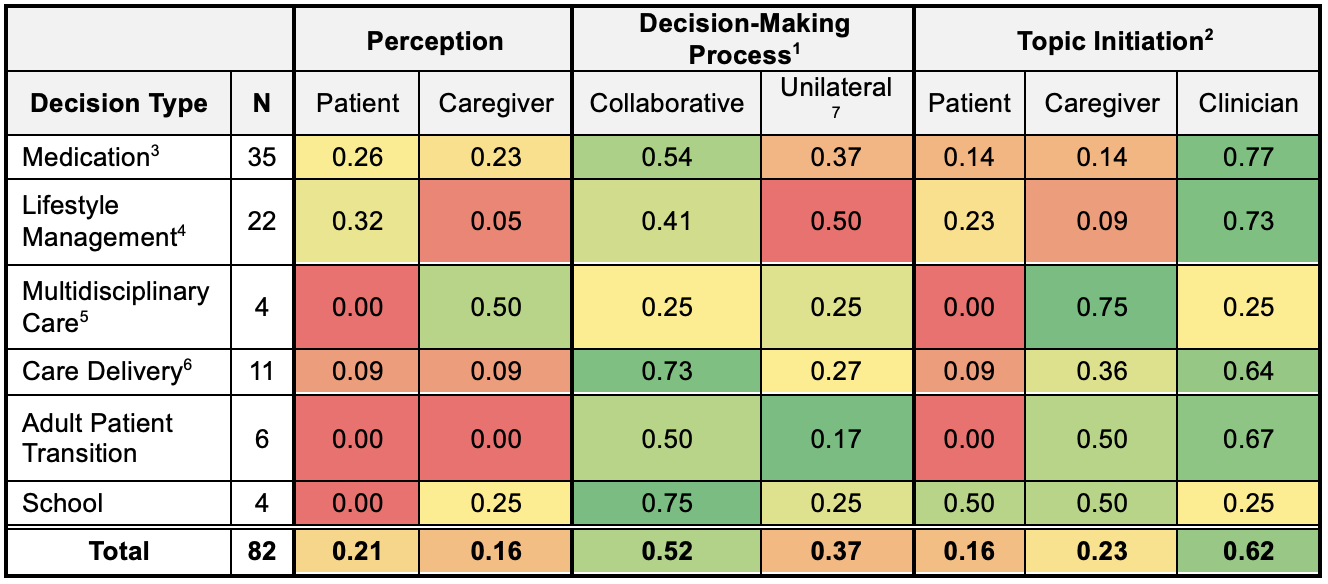
Objective: We aimed to understand CDM from the perspectives of CKD youth and their caregivers by analyzing the decisions and decision-making practices utilized during routine outpatient clinic encounters. Specifically, we evaluated how often patients and caregivers (1) perceive when a decision is made, (2) participate in decision-making, and (3) bring up decision topics.
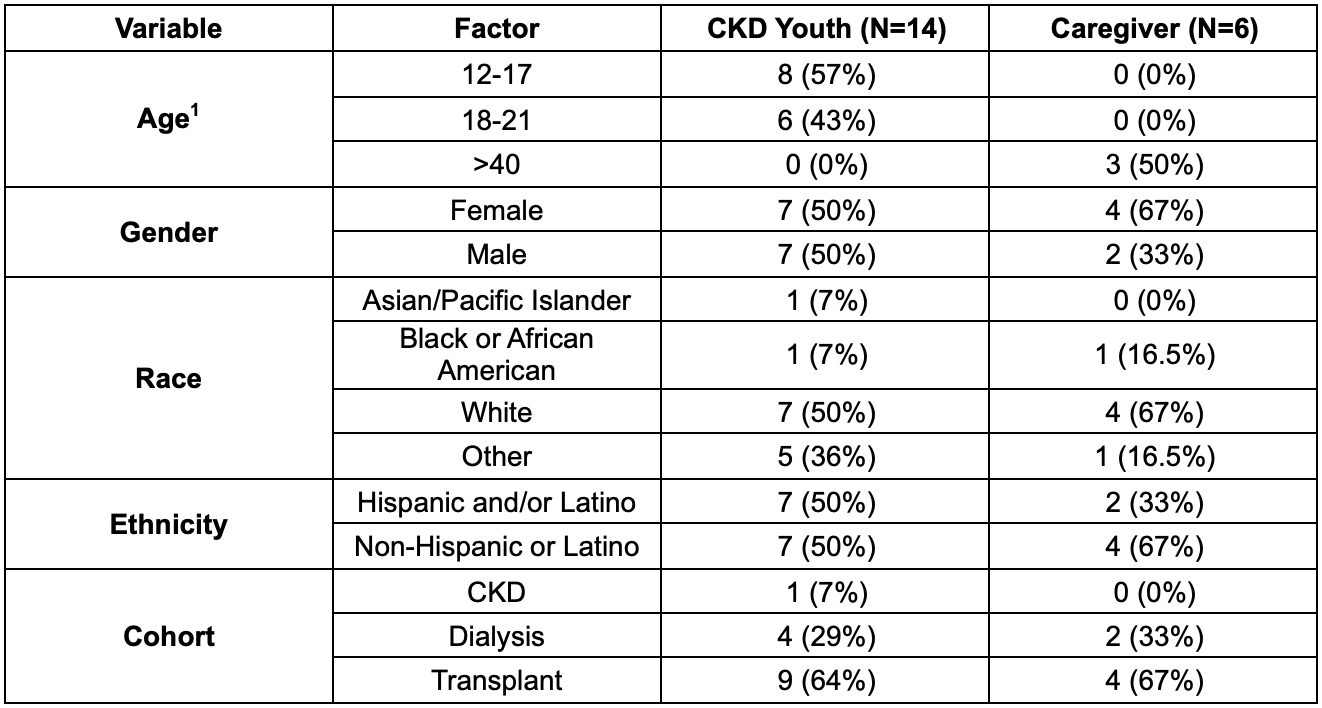
Design/Methods: We conducted observations of nephrology clinic visits and follow-up interviews with CKD youth (age 12-21) and their caregivers at a single academic children’s hospital. During the observations, the study team (1) identified (total count) & categorized all decisions made, (2) who participated in the decision-making process, and (3) who brought up the decision topic. In the post-encounter interview, participants were asked to describe what decisions they remember being made during the visit and if they agreed with them. The observations and interviews were audio recorded, transcribed, and analyzed through content analysis.
Results: Participant details are in Table 1. 82 decisions were observed over 14 encounters. Patient and caregiver perceptions of decisions made in a clinic visit were low in frequency compared to researcher observation, despite 52% of the decisions made being collaborative (Table 2). 50% of the lifestyle management decisions were unilaterally made by clinicians, who brought up the most decision topics during the observed visit.
Conclusion(s): Our study suggests multiple opportunities for improving CDM in pediatric nephrology, such as developing interventions that increase perception rates and limit unilateral decision-making by clinicians. These interventions should promote and support patients to become empowered to introduce decisions, share their values, and engage in CDM. Also, they should encourage clinicians to create further opportunities for CDM within the clinical encounter. These preliminary findings highlight the importance of further study of decision-making in this population to facilitate patients’, parents’, and clinicians’ engagement in CDM.