Neonatology
Session: Neonatal Quality Improvement 6
89 - Birth Time and Early Outcomes in Very Preterm Infants in China: A Cohort Study
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 89
Publication Number: 89.2768
Publication Number: 89.2768

Si Chen, MA (she/her/hers)
pediatric physician
The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University
Wenzhou, Zhejiang, China (People's Republic)
Presenting Author(s)
Background: China currently lacks comprehensive national-level data regarding the birth timing and outcomes of very preterm infants (VPIs).
Objective: To investigate the correlation between the timing of birth and the outcomes of VPIs in China, and furnish crucial data to improve the quality of perinatal care.
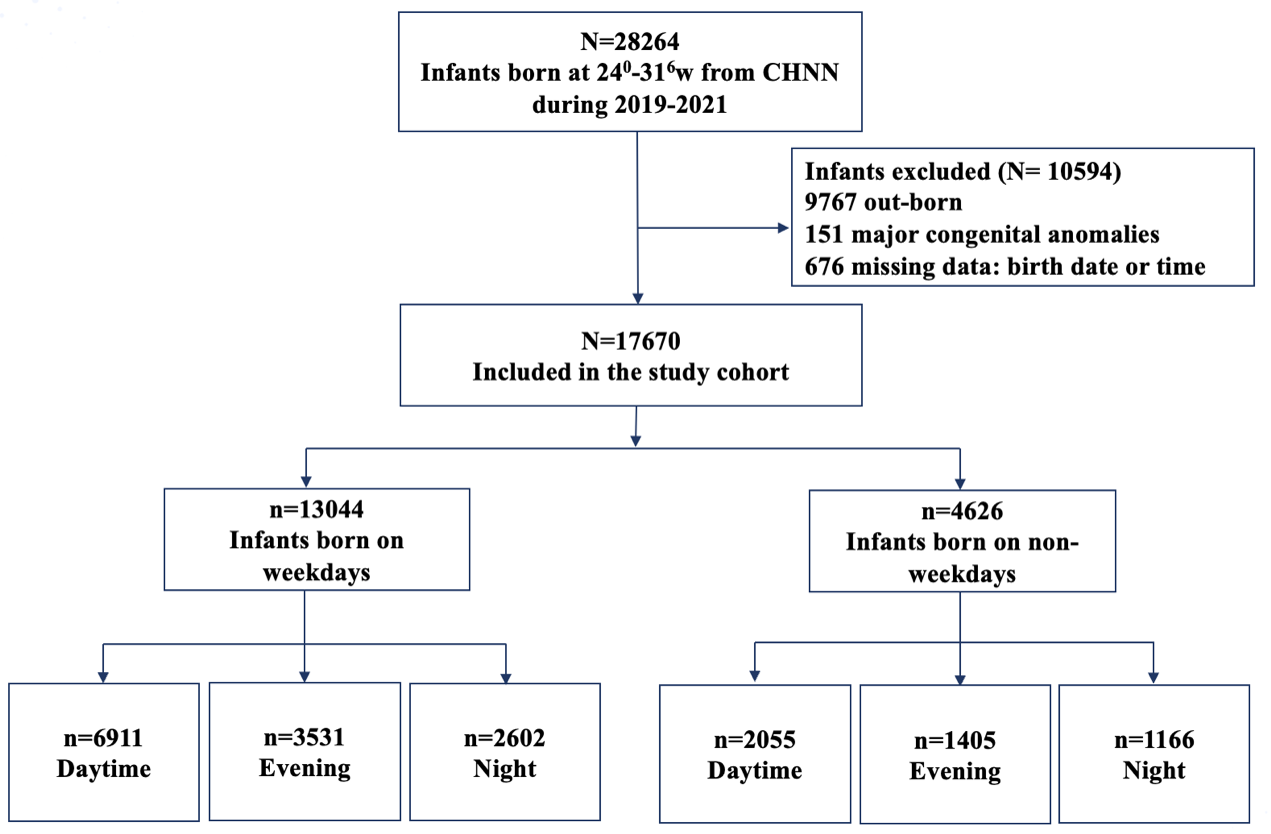
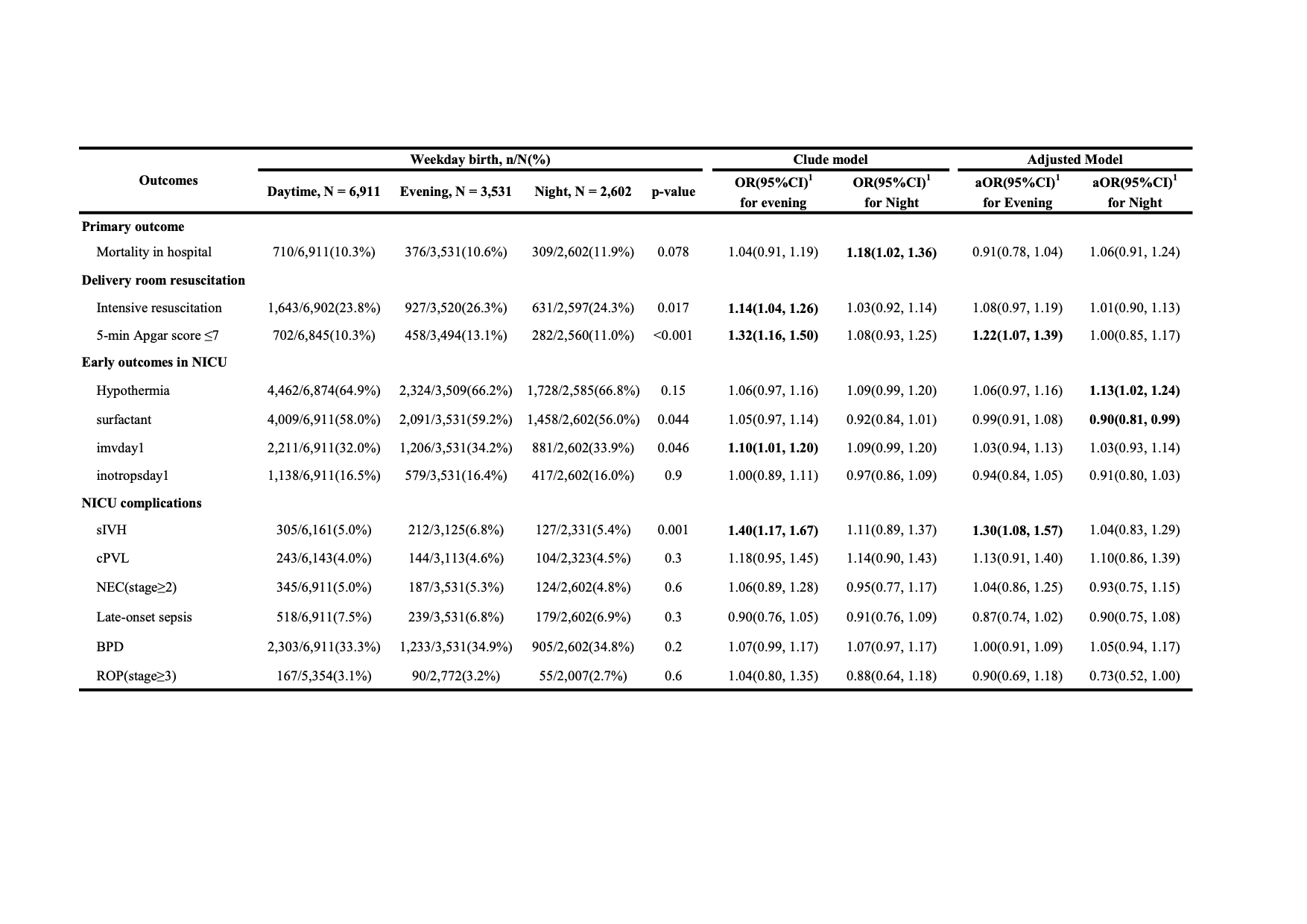
Design/Methods: This retrospective cohort study was conducted based on Chinese Neonatal Network (CHNN). Infants with a gestational age (GA) of < 32 weeks who were admitted to NICUs between January 1, 2019, and December 31, 2021 were included. Infants who were out-born or had major congenital anomalies were excluded. The primary outcome was in-hospital mortality rates. Secondary outcomes encompassed various aspects of neonatal care and morbidity within the delivery room and NICUs, including intensive resuscitation, 5-minute Apgar scores ≤7, admission hypothermia (T < 36.5°C), severe intraventricular hemorrhage (sIVH, grade ≥3), etc. Confounding variables included maternal perinatal complications, infants GA and small for gestational age. Multivariable logistic regression models and generalized additive models were employed to evaluate the relationships between outcomes and birth time. A stratified analysis was conducted based on GA or delivery type.
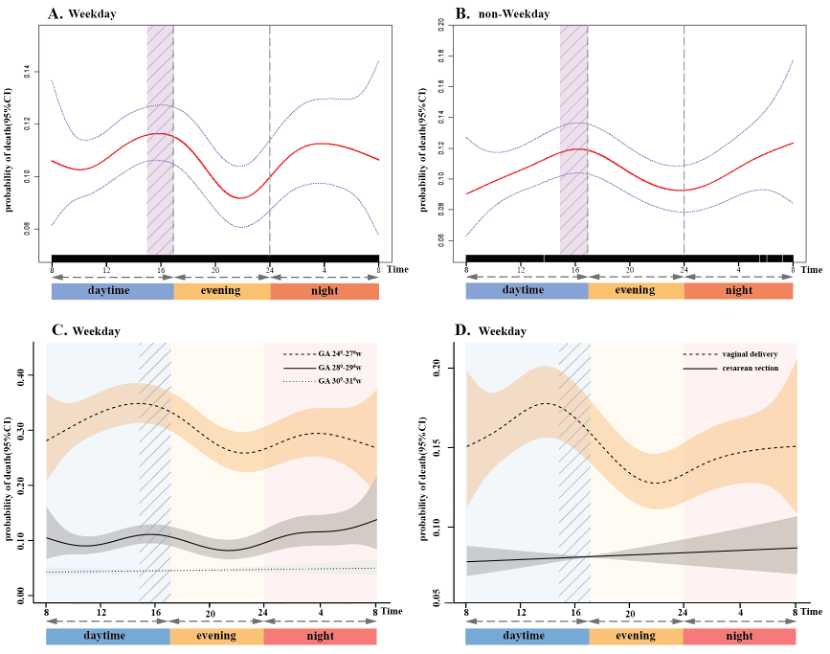
Results: In 17,670 VPIs, we identified a distinct dual-peak pattern characterized by a "handover effect" of mortality elevation during the transition between the daytime-evening shift, as well as the night shift among infants born on weekdays. Infants at 240-276 weeks GA were identified as a crucial subgroup. There was a persistent association between evening births and 5-minute Apgar scores ≤7 (adjusted odds ratio [aOR] 1.22, 95% confidence interval [CI] 1.07 to 1.39) or sIVH (aOR 1.30, 95% CI 1.08 to 1.57). Infants born at night were also more prone to experiencing hypothermia (aOR 1.13, 95% CI 1.02 to 1.24). Among infants with a GA of 280-296 weeks, the association between the night shift and intensive resuscitation (aOR 1.23, 95% CI 1.02 to 1.48), as well as evening shift and 5-minute Apgar scores ≤7 (aOR 1.38, 95% CI 1.11 to 1.71), remained statistically significant. In cases of infants at 300-316 weeks GA, the risk of sIVH significantly increased during the evening shift (aOR 1.78, 95% CI 1.27 to 2.48).
Conclusion(s): The “handover effect” during daytime-evening shift and a nighttime peak have been identified, particularly impacting infants at 240-276 weeks GA. Infants born of 280-316 weeks GA during off-peak hours are associated with a heightened risk of complications such as asphyxia, hypothermia, or sIVH.