Critical Care
Session: Critical Care 1
104 - Comparing the indications and outcomes of pediatric patients requiring continuous renal replacement therapy alone and in tandem with extracorporeal membrane oxygenation
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 104
Publication Number: 104.2762
Publication Number: 104.2762

Salvador R. Maffei, MD (he/him/his)
Clinical Fellow
Baylor College of Medicine
HOUSTON, Texas, United States
Presenting Author(s)
Background: Continuous renal replacement therapy (CRRT) allows for slow fluid removal and solute clearance in critically ill pediatric patients. The most common indications for CRRT are fluid overload, acute kidney injury (AKI), and clearance of ammonia or other toxins. CRRT can be prescribed as a solitary or in tandem with other extracorporeal therapies, including extracorporeal membrane oxygenation (ECMO). Acute kidney injury (AKI) has been reported in 42-85% of pediatric patients requiring ECMO, most commonly occurring in the first 48 hours of therapy.
Objective: We aim to compare the indications and outcomes of patients who require CRRT alone to those who require CRRT in tandem with ECMO.
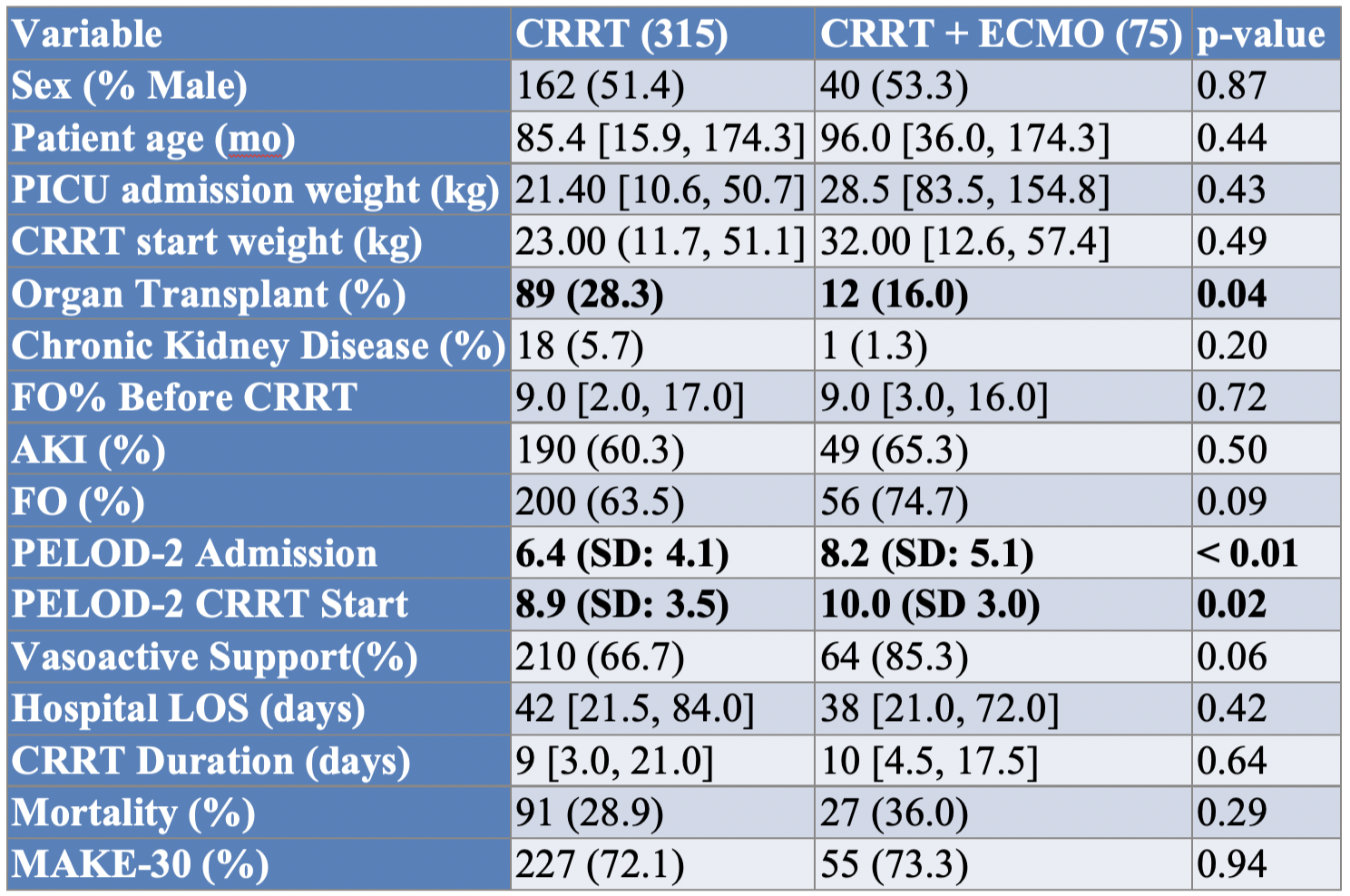
Design/Methods: We conducted a retrospective dual-center study of children and young adults (age < 26 years) admitted to the pediatric or cardiac intensive care unit between February 2014 to February 2020. Illness severity was measured using pediatric logistic organ dysfunction (PELOD-2) score. We collected net fluid balance (NFB) and urine output (UOP) for the first three days of CRRT. Our primary outcome was major adverse kidney events at 30 days (MAKE-30).
Results: 390 patients were included, with 315 patients (81%) requiring CRRT alone and 75 (19%) requiring both ECMO and CRRT. In the CRRT cohort, the most common comorbidity was hematology or oncology in 82 patients (26%), while cardiovascular comorbidities were most common in the ECMO cohort (28 patients, 37%). The most common admission diagnosis for the CRRT cohort was sepsis (79 patients, 25%), and shock other than sepsis was most common in the ECMO cohort (23 patients, 31%). The median PELOD-2 score at CRRT initiation was 8.89 and 9.95 (p < 0.02) in the CRRT and ECMO cohorts, respectively. 151 (48%) of CRRT alone achieved negative NFB, compared with 25 (33%) of the patients requiring ECMO (p=0.03). Median UOP over 72 hours was 0.31 mL/kg/hr and 0.22 mL/kg/hr for the CRRT and ECMO cohorts, respectively (p < 0.01). MAKE-30 occurred in 227 patients (72%) and 55 patients (73%) in the CRRT and ECMO cohorts, respectively (p=0.94).
Conclusion(s): There were significant differences in the primary comorbidity, PELOD-2 at CRRT start, and reason for ICU admission in patients who require CRRT alone compared to both ECMO and CRRT. Although the CRRT cohort was more likely to achieve negative NFB and maintain higher UOP over the first 3 days of CRRT, the incidence of MAKE-30 did not differ. Future studies should investigate rates of fluid removal and other possible modifiable factors associated with MAKE-30 in children requiring CRRT.
.png)
.png)
