Neonatology
Session: Neonatal Quality Improvement 4
57 - An intervention to improve kangaroo care (KC) education and time to first KC among premature infants in the neonatal intensive care unit (NICU)
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 57
Publication Number: 57.2761
Publication Number: 57.2761

Alicia Lore, MD Candidate (she/her/hers)
MS3
McGovern Medical School at the University of Texas Health Science Center at Houston
Houston, Texas, United States
Presenting Author(s)
Background: Kangaroo Care (KC) provides an optimal care environment supportive of neonatal quality measures including improved survival, thermal regulation, cardiorespiratory stability, lower pain scores, and reduced infection. Despite known KC benefits, protocols are not widely implemented due to various barriers specific to individual institutions. This group previously described delays in time to first KC in preterm infants due to gaps in provider knowledge and training.
Objective: We hypothesize KC provider education intervention will improve time to first KC across PT infants in the NICU.
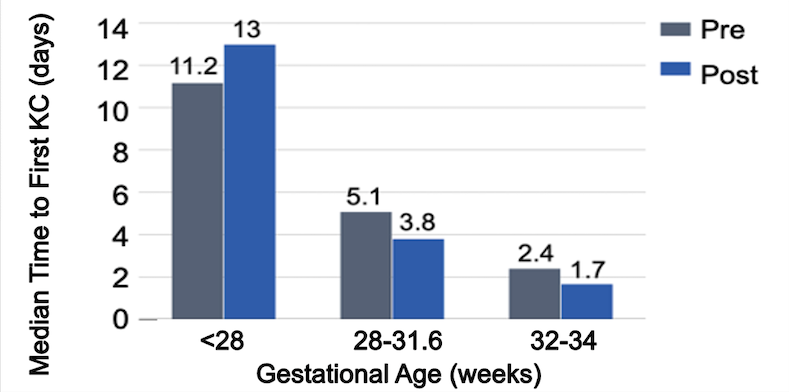
Design/Methods: This single site quality improvement (QI) study includes inborn infants 22-34 weeks gestation at Children’s Memorial Hermann Hospital (CMHH). A 2018 cohort was used for pre-intervention baseline data. Post-intervention data was collected from June to August 2023. Median time to first KC was analyzed across 3 subgroups in both cohorts: < 28 weeks extremely preterm infants (EP), 28-316/7 weeks preterm infants (PT1) and 32-34 weeks preterm infants (PT2). Educational posters, bedside calendars, and signs distributed in the NICU and via email targeted provider education and awareness. The primary outcome variable was time to first KC, analyzed using descriptive statistics.
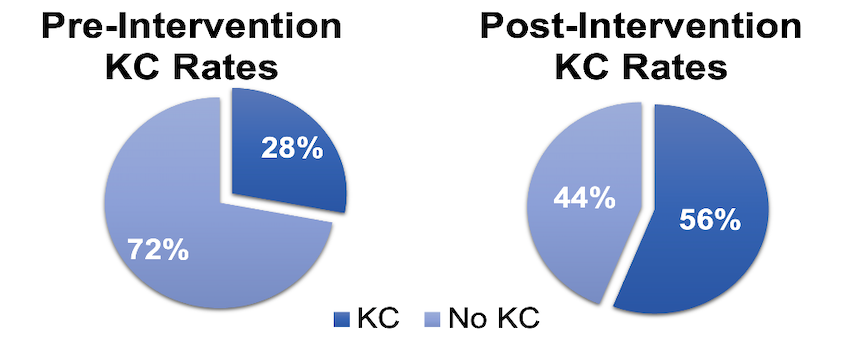
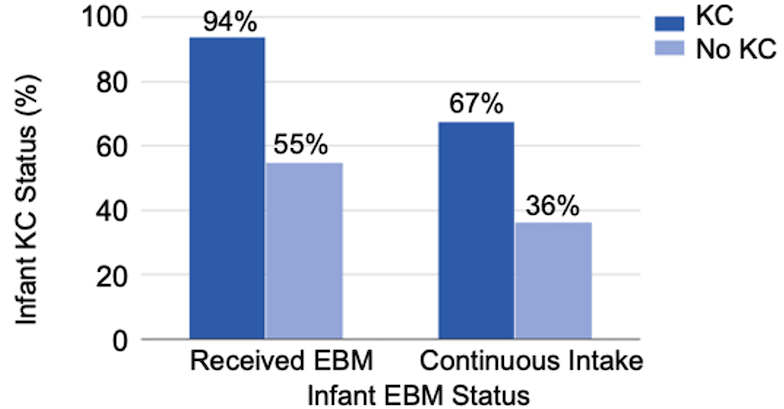
Results: Post-intervention median time to first KC decreased from 5.1 to 3.8 days (d) and 2.4 to 1.7d in PT1 and PT2 infants, respectively. Median time increased in EP infants from 11.2 to 13d. Overall, KC performance across all infants doubled post-intervention (28% to 56%). 94% of infants receiving KC also received EBM, compared to 55% of infants receiving no KC. Similarly, KC correlated with higher rates of mothers who continued to pump until infant discharge from NICU (67% +KC versus 36% no KC).
Conclusion(s): Educational interventions improved rates of KC across all infants and decreased time to first KC within subgroups PT1 and PT2. Higher 2023 NICU census with increased workload among a younger nursing staff may account for decreased KC facilitation in the more vulnerable subgroup of EP infants. There is a positive and significant correlation between KC and EBM production, and a positive correlation between KC and continuous EBM provision throughout NICU course to infant discharge. Findings support our hypothesis that KC awareness and education play a vital role in ensuring optimal wellbeing of infants and families. Future QI efforts focused on parental education and implementation of an early, standardized KC unit protocol is warranted.