Neonatology
Session: Neonatal General 7: Respiratory
240 - Effect of Less Invasive Surfactant Administration on Neonatal Fellows' Intubation Opportunities and Direct Laryngoscopy Intubation Skills.
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 240
Publication Number: 240.2810
Publication Number: 240.2810
- OP
Olena Predtechenska, MD (she/her/hers)
Neonatologist
Cohen Children's Medical Center
New Hyde Park, New York, United States
Presenting Author(s)
Background: Neonatal tracheal intubation (TI) is a critical skill in neonatology. There is a potential threat to the skill acquisition among neonatal trainees due to changes in neonatal practice, such as management of the infants born through meconium-stained fluid, emphasis on non-invasive respiratory support, and less invasive surfactant administration (LISA) technique. Little is known about the effect of these changes on TI skills in the academic setting. In January 2021, LISA with videolaryngoscopy (LISA+VL) was introduced as a primary method for surfactant delivery in our level 3 and 4 NICUs. TIs continued to be done via direct laryngoscopy.
Objective: 1. Study the effects of LISA+VL on overall TI number and rate.
2. Study effects of LISA+VL on trainees' TI skills.
Design/Methods: We conducted a retrospective chart review of ventilated patients admitted to the 2 main NICUs from 1/1/2020 to 12/31/2020 (prior to LISA+VL) and from 1/1/2022 to 12/31/2022 (1 year after LISA start day). We reviewed endotracheal airway placement documentation. Patients transported from an outside NICU intubated, intubated by non-neonatal providers, those with airway anomalies, or those without airway placement documentation were excluded. We recorded the training level of the first airway provider, number of TI attempts, and success of TI or the need for escalation to a senior provider. Statistical analysis was performed using independent samples T-test and Chi squared analysis.
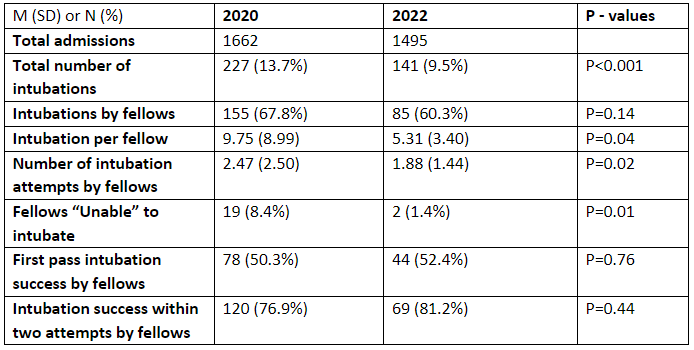
Results: Total number of captured direct laryngoscopy TIs decreased by 38 % after LISA +VL which significantly changed TI events per admission per year from 13.7 to 9.5 (p < 0.001) despite similar overall NICU admissions. The proportion of TIs performed by fellows was unchanged, 67.8% vs 60.3%, p=0.14. The average number of TIs performed per fellow per year significantly decreased from 9.75 to 5.31, p=0.04. The average number of TI attempts to a successful intubation by a fellow decreased from 2.47 to 1.88, p=0.02. The number of instances when a fellow was unable to successfully complete an TI and required escalation decreased from 8.4% to 1.4%, p=0.01.
Conclusion(s): The significant decrease in number and rate of TIs due to introduction of LISA+VL did not have a negative impact on fellows’ direct laryngoscopy TIs skills and remained consistent with prior literature. In fact, trainees required fewer attempts to perform a successful TI with decreased rate of escalation to a senior provider. We speculate that this is due to wide use of videolaryngoscopy for LISA, that provides similar if not better teaching and training opportunities in clinical settings.