Neonatology
Session: Neonatal Neurology 4: Clinical
520 - Neurodevelopmental and Neurobehavioral Outcomes at 2 Years of Age in Extremely Premature Infants with Bronchopulmonary Dysplasia
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 520
Publication Number: 520.1309
Publication Number: 520.1309

Semsa Gogcu, MD, MPH (she/her/hers)
Clinical Associate Professor
Wake Forest School of Medicine of Wake Forest Baptist Medical Center
Winston Salem, North Carolina, United States
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD) remains a common complication with an increased risk of mortality and long-term morbidity in extremely premature (EP, < 28 weeks of gestation) infants. While many studies demonstrated a clear increase in the risk of neurodevelopmental impairment, particularly in those with more severe BPD, few studies included neurobehavioral outcomes.
Objective: To compare the neurodevelopmental and neurobehavioral outcomes of EP infants with BPD to infants without BPD in the Preterm Erythropoietin Neuroprotection (PENUT) Trial.
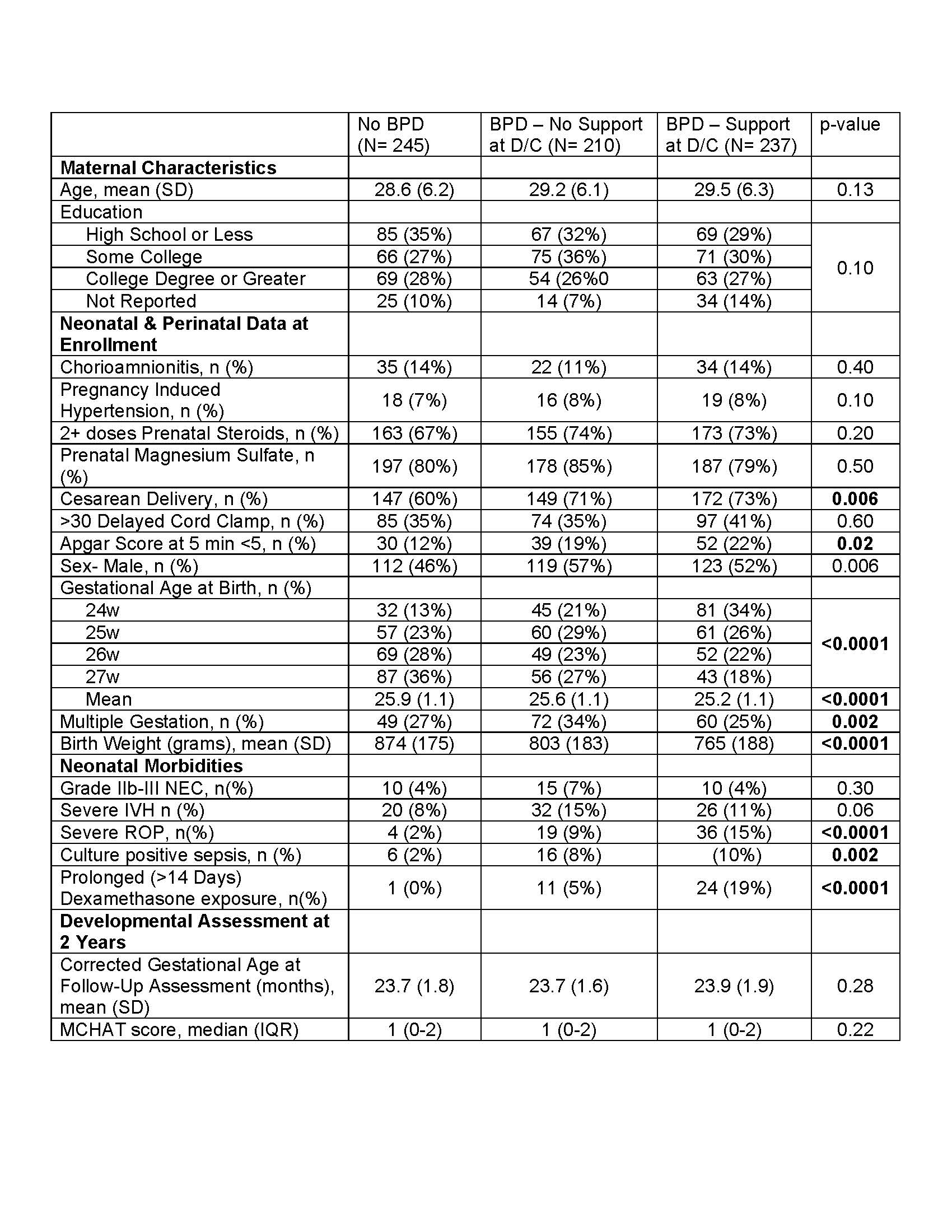
Design/Methods: This post-hoc analysis of PENUT data included infants born 24 0/7-27 6/7 weeks’ gestational age who were diagnosed with BPD and completed 1 or more subscales of the Bayley Scales of Infant Development, 3rd edition (BSID-III), Modified Checklist for Autism in Toddlers (MCHAT), and the Child Behavior Checklist (CBCL) at 2 years corrected age. Infants with BPD were further separated by need for respiratory support at discharge as a proxy of BPD severity. Results were compared across groups using generalized estimating equations (GEE) models to account for correlation between siblings, and were adjusted for common comorbidities. Linear models were used for BSID-III and MCHAT, and logistic regression models were used to assess odds of borderline (score>64) or clinical (score>70) T-scores for the CBCL subscales.
Results: 692 infants were included, 447 (65%) were diagnosed with BPD. Of those, 237 (53%) required respiratory support at discharge. Infant characteristics are summarized in Table 1. Infants with BPD regardless of respiratory support at discharge had lower BSID-III motor scores than infants without BPD (Figure 1). There was no association between the severity of BPD at discharge and MCHAT-R or CBCL scores. No differences were found between groups on MCHAT (Table 1) or in any CBCL subscale (Figure 2).
Conclusion(s): This post-hoc analysis of a contemporary cohort of extremely preterm infants demonstrates that while BPD is still associated with worse motor scores, it does not appear to be linked to neurobehavioral outcomes at 2 years corrected age after adjusting for important clinical confounders. Although results should be interpreted with caution given the post-hoc study design, our findings imply that the concern for a negative impact of BPD on neurobehavior may be negligible.
.jpg)
.jpg)
