Environmental Health
Session: Environmental Health
240 - Seasonal Variation In Blood Pressure Severity At Initial Visit With Subspecialist For Youth With Hypertension Disorders
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 240
Publication Number: 240.1398
Publication Number: 240.1398

Carol Vincent, MD (she/her/hers)
pediatric nephrology clinical instructor
Wake Forest School of Medicine of Wake Forest Baptist Medical Center
Winston Salem, North Carolina, United States
Presenting Author(s)
Background: Blood pressure (BP) in youth and adults is higher in colder months, lower in warmer months. The impact of this seasonal variation on BP severity and cardiovascular (CV) health in youth with hypertension (HTN) disorders remains unknown. Thus, addressing this knowledge gap has implications for guidelines, diagnosis, and management of youth with HTN disorders and is instrumental to interpreting and implementing management of HTN disorders in youth at a population level.
Objective: Determine the association of season with BP severity and prevalence of CV health factors (CVHF) and target organ injury (TOI). We hypothesized that BP would be higher in cooler months (Winter), CVHF and TOI prevalence would remain stable throughout the year, and sex would modify these associations.
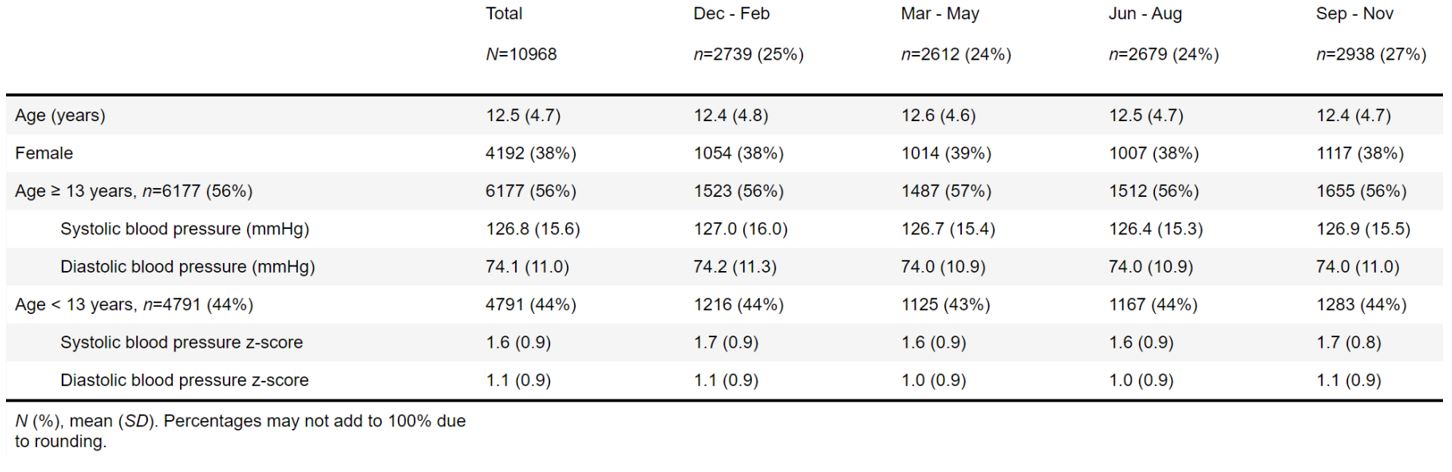
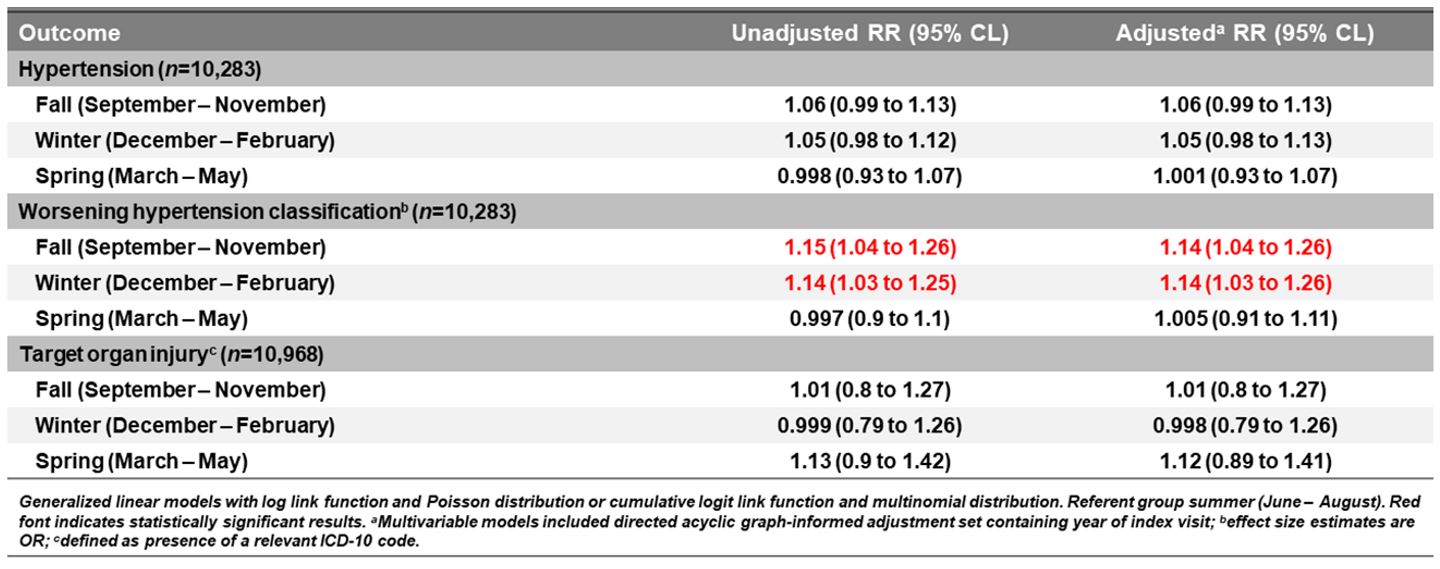
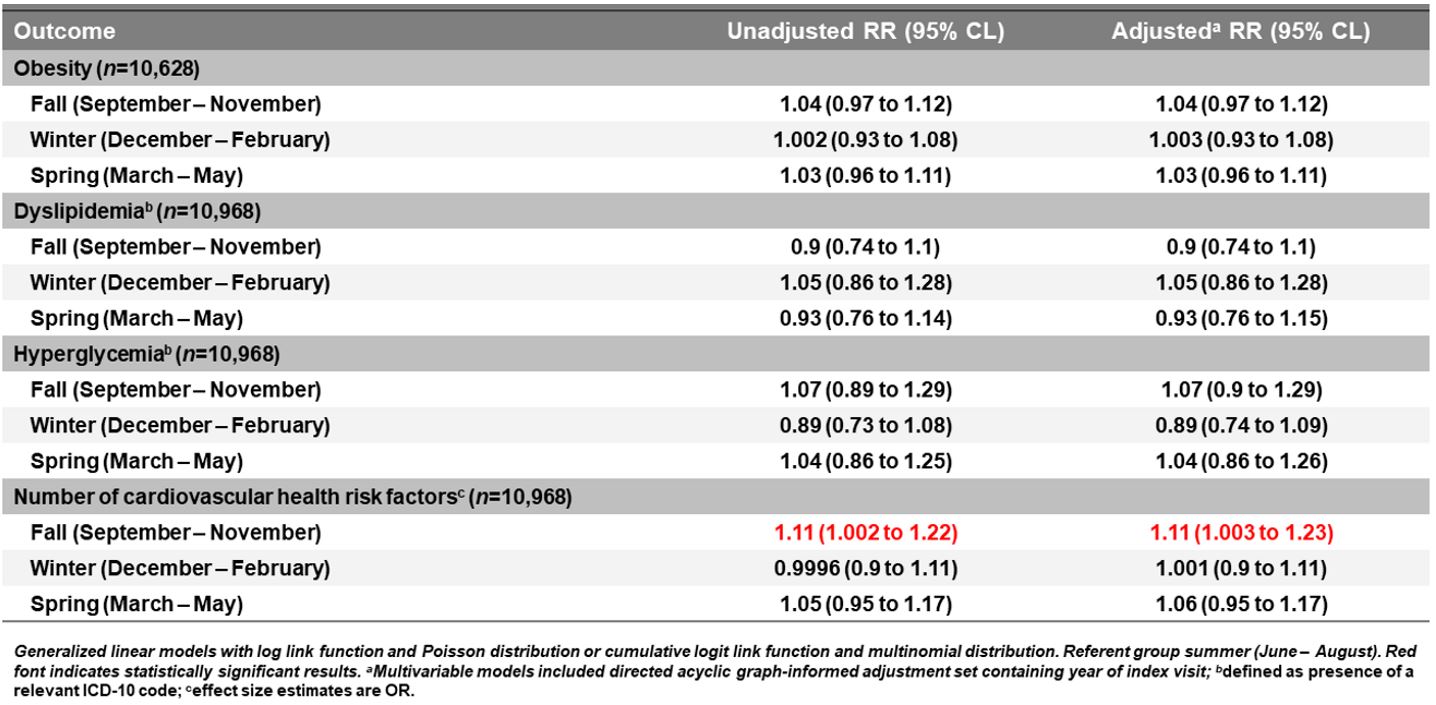
Design/Methods: Cross-sectional analysis of baseline EHR data from youth referred for HTN disorders in the multisite retrospective SUPERHERO Registry. Inclusion criteria were age < 19 years and index subspecialty clinic visit for HTN disorders by ICD-10 codes from 1/1/2015–12/31/2022. Exclusion criteria were dialysis, kidney transplantation, or pregnancy by ICD-10 codes. Our exposure was season (Winter: Dec-Feb, Spring: Mar-May, Summer: Jun-Aug, and Fall: Sep-Nov) of index visit to subspecialist for HTN. Our outcome was BP severity by national guidelines, prevalence of CVHF (obesity by BMI percentile, dyslipidemia and hyperglycemia by ICD-10 code), total number of CVHF (0-3), and TOI presence (by ICD-10 code). We used generalized linear models stratified by sex and adjusted for geographic region.
Results: Of 10,968 participants, 38% were female and average age was 12.5 years (SD 4.7) (Table 1). Compared to Summer, Fall and Winter were associated with higher systolic BP (β 1.05; 95% CL [0.14, 1.96] and β 1.43; 95% CL [0.5, 2.35]) in adolescents and risk of more severe HTN classification (RR 1.14; 95% CL [1.04, 1.26]; RR 1.14; 95% CL [1.03, 1.26], Table 2). Fall was associated with higher risk of total CVHF (RR 1.11; 95% CL [1.003, 1.23], Table 3). Season was not associated with TOI (Table 2) or other BP measures. There was a sex difference in Spring and BP severity with male sex associated with lower systolic BP z-score and female sex with worse BP classification.
Conclusion(s): BP severity and CVHF prevalence in youth at index visit to a subspecialist for HTN disorders varied across seasons with evidence of effect modification by sex. Season of assessment should be considered when making management and follow up decisions for this population especially for individuals with high CV or TOI risk.