Critical Care
Session: Critical Care 1
117 - Palliative Care and Brain Death: Variability in Palliative Care Consultation and Discharge Disposition in a National Sample
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 117
Publication Number: 117.3246
Publication Number: 117.3246
- FC
Francesca M. Chu (she/her/hers)
Medical Student
University of Chicago Pritzker School of Medicine
Chicago, Illinois, United States
Presenting Author(s)
Background: Understanding and accepting death by neurological criteria is profoundly challenging for families of pediatric patients. One source of support may include palliative care providers, whose focus on compassionate communication and expertise in end-of-life issues make them uniquely well suited to supporting families through brain death diagnoses. However, factors associated with receiving palliative care consultation (PCC) prior to brain death are not well characterized. Similarly, there is little known about characteristics of patients who are not discharged as expired despite their brain death diagnosis, which may represent a family request for continuation of technological support.
Objective: To investigate demographic and clinical characteristics associated with PCC and having discharge disposition other than “expired,” among pediatric patients declared dead by neurological criteria.
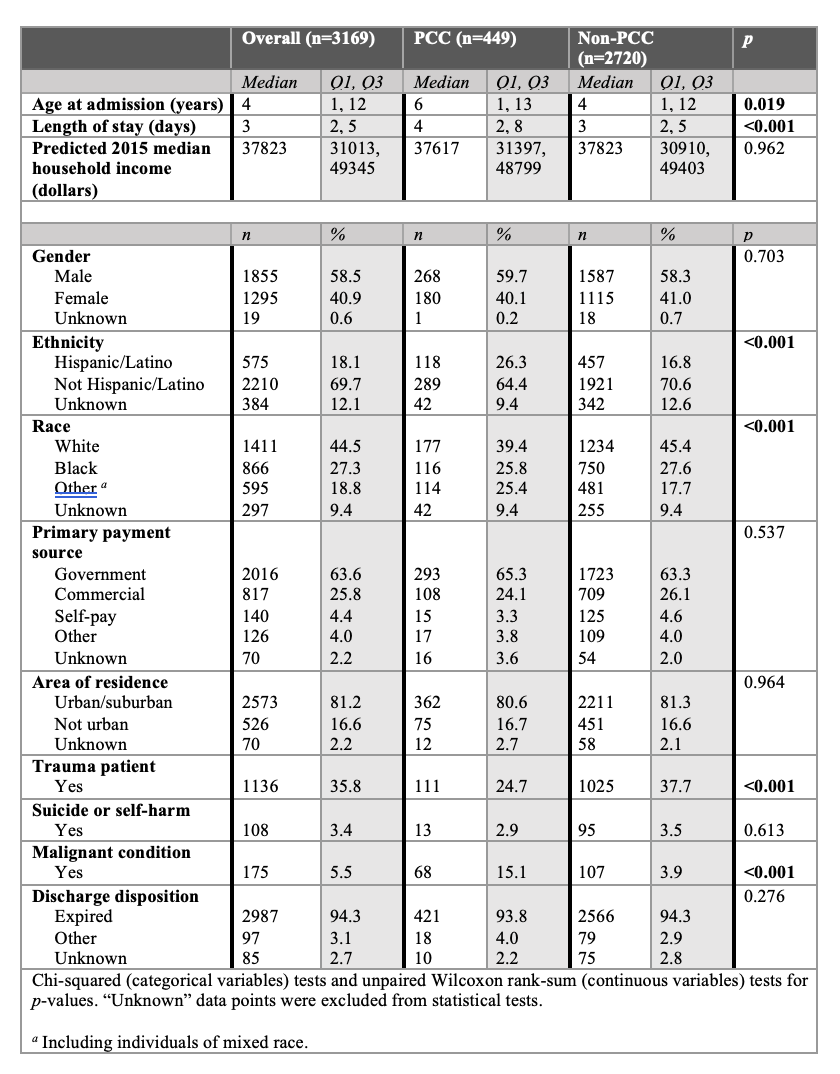
Design/Methods: A retrospective cohort study was performed using data from 44 tertiary pediatric hospitals in the United States, within the Pediatric Health Information System (PHIS) database. Patients included in the study were those ages 21 and younger, declared dead by neurological criteria, and discharged between October 1, 2015, and December 31, 2022. Generalized linear mixed effects models were developed to examine characteristics associated with PCC or not being discharged as expired.
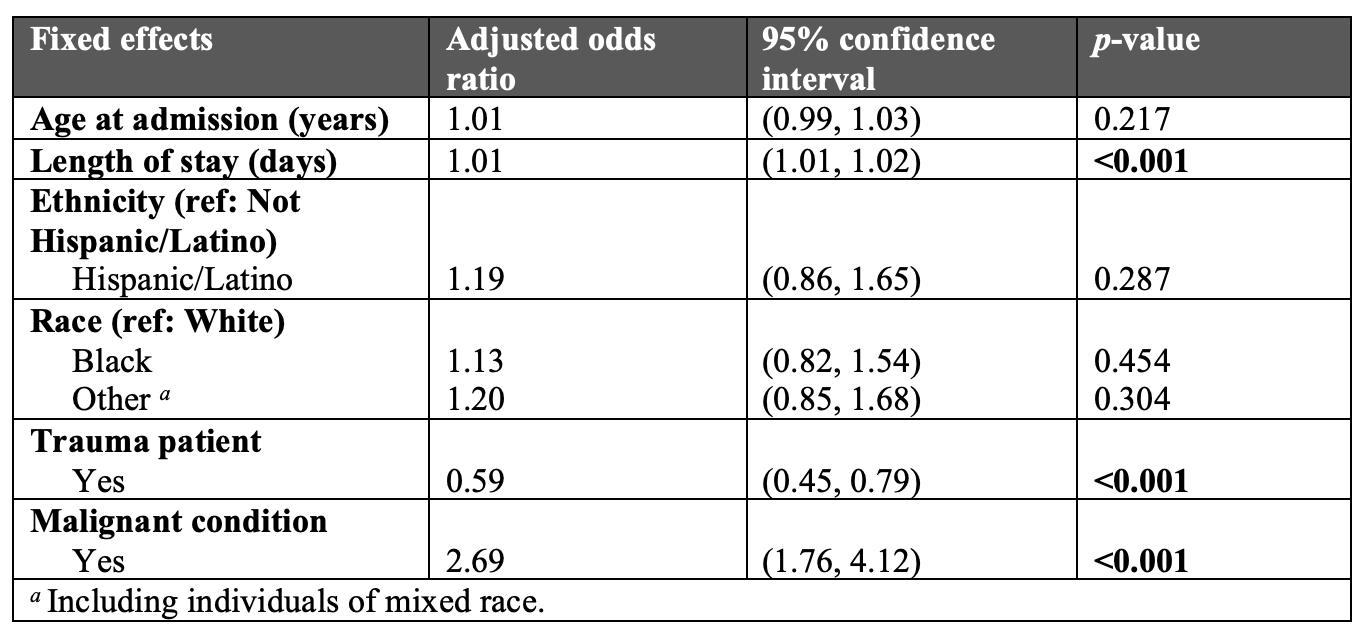
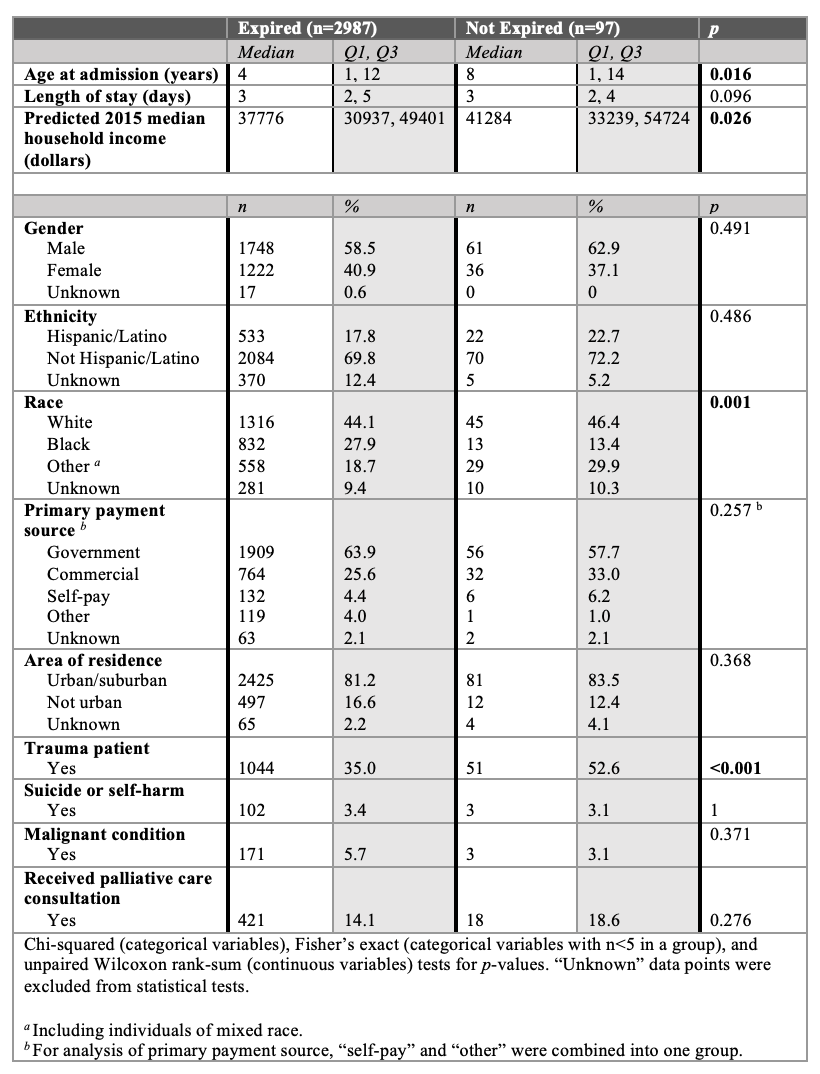
Results: Of 3169 patients studied, 14.2% (n = 449) received PCC and 2.3% (n = 97) were not discharged as expired. Across hospitals, the percentage of patients receiving PCC ranged from 0% (2 hospitals) to 80.0% (median 11.0%, IQR 13.9%); the percentage of those not discharged as expired ranged from 0% (22 hospitals) to 33% (median 0.4%, IQR 3.9%). PCC was associated with longer stay in days (aOR 1.01, 95% CI 1.01–1.02, p < 0.001) and malignant condition (aOR 2.69, 95% CI 1.76–4.12, p < 0.001), and negatively associated with trauma (aOR = 0.59, 95% CI 0.45–0.79, p < 0.001). Not being discharged as expired was twice as likely in trauma than non-trauma patients (aOR 2.00, 95% CI 1.22–3.26, p < 0.006), and less likely in Black than White patients (aOR 0.34, 95% CI 0.17–0.68, p < 0.002).
Conclusion(s): Longer stay and malignant condition were associated with PCC, while PCC was less used in trauma cases. Not being discharged as expired was more common in White than Black patients, and in trauma cases. The study highlights the need for further research on potential benefits of palliative care in brain death cases, including for trauma patients.