Emergency Medicine
Session: Emergency Medicine 2: Operations
368 - Retrospective Evaluation of a Novel Post-Event Debriefing Tool to Identify Emotional Impact and Actionable Action Ideas at 2 Pediatric Emergency Departments
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 368
Publication Number: 368.123
Publication Number: 368.123

Leslie A. Hueschen, MD (she/her/hers)
Pediatric Emergency Medicine Physician
University of Missouri-Kansas City;Children's Mercy Hospital
KANSAS CITY, Missouri, United States
Presenting Author(s)
Background: The American Heart Association recommends debriefing after resuscitation. Many pediatric emergency departments(ED) recognize the need for formal debriefing but lack the process or training. Studies demonstrate how debriefing identifies areas of improvement but little is known about their emotional impact.
Objective: We describe a novel debriefing process and it's impact on emotional response and in identifying improvement ideas. We also studied duration of debrief, effect on ED flow, and involved staff.
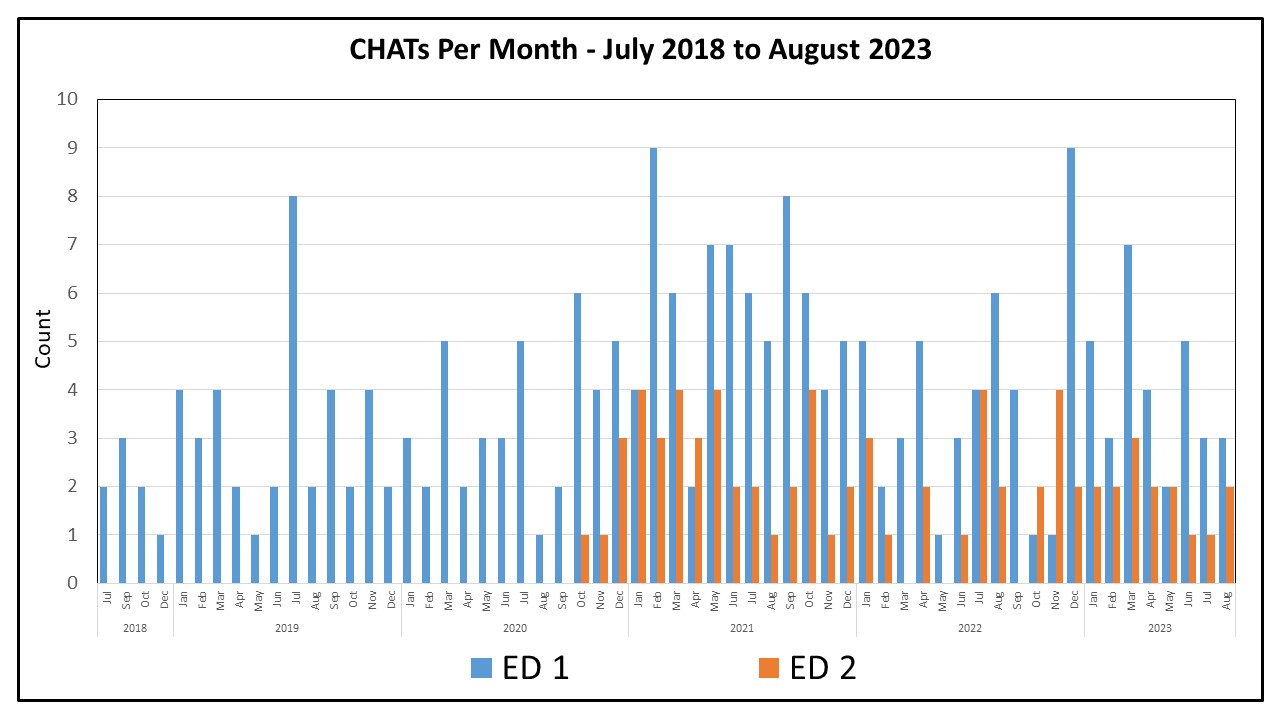
Design/Methods: A multidisciplinary workgroup developed a debrief tool-Critical Huddle After Treatment(CHAT)-with implementation in 2018. The ED consists of 2 sites: an urban quaternary ED1(67,000 patients/year) and a community-based ED2(45,000 patients/year). We started implementation in ED1 in July 2018 and expanded to ED2 in October 2019. We retrospectively analyzed data from July 2018-August 2023. CHAT variables included location, indication, attendance, and reason for not performing a CHAT. We studied the number of actionable items identified, CHAT leaders assessment of engagement, and self-reported reactions pre- and post-CHAT(red-highly confused/conflicted, yellow-confused, green-no concerns). We also studied the impact on ED flow, CHAT duration, and the perceived effect on ED flow.
Results: Of the CHATs initiated, 71% were completed(303/429). Once the program was fully implemented, 8.77/month were completed(Fig 1). Mean CHAT duration was 21 minutes and participants included bedside nurse(66%), attending(61%), recording nurse(53%), care technician(50%), charge nurse(44%), respiratory therapist(44%), resident(39%), pharmacist(35%), fellow(32%), social worker(12%), and surgeon(4%). Leading indications for CHAT were medical resuscitation or trauma. Of respondents, 71% did not think debriefing significantly impacted the ED flow. The primary reasons noted for abstaining from a CHAT included “ED too busy”(41%), “not necessary"(24%), or not answered(23%).
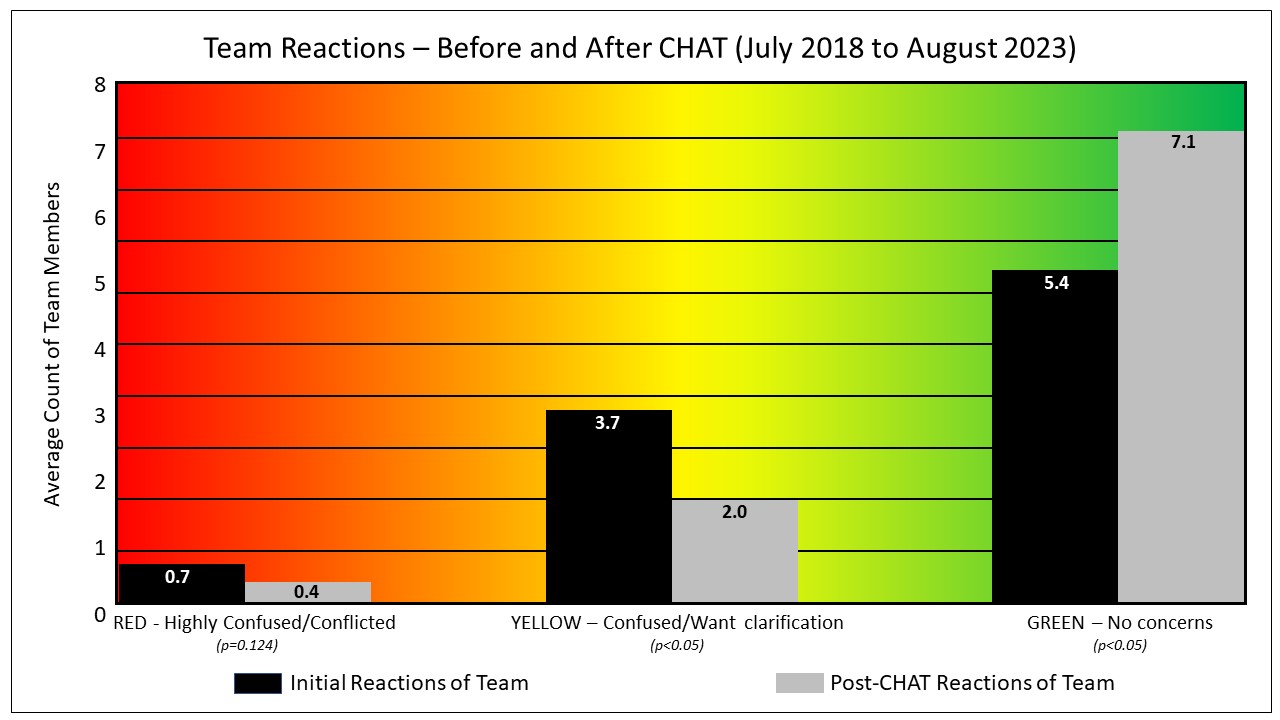
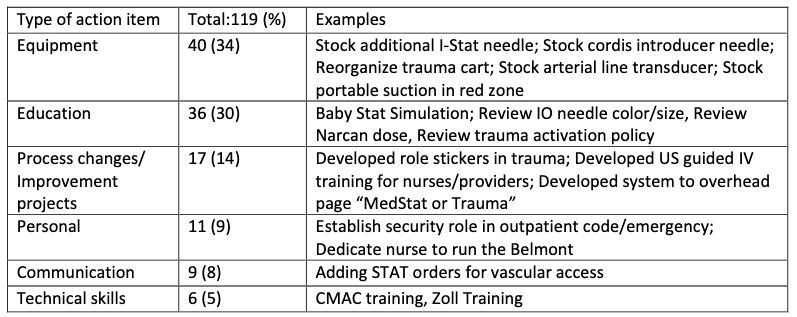
The majority(91%) of participants were highly or moderately engaged in the CHAT. Self-reported reactions improved after the CHAT; with decreasing ‘yellow’ participants(p < 0.05) and increasing ‘green’(p < 0.05) post-debrief.(Fig 2) The decrease in ‘red’ participants was not statistically significant (p=0.124).(Fig 2) From the 303 CHATs performed, the team identified 119 actionable items.(Table 3)
Conclusion(s): The CHAT process allows teams to effectively debrief after a critical event without impacting ED flow and shows improvement in staff emotional reactions. Multiple areas of improvement were identified, leading to many institutional process changes.