Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 2: BPD and prematurity
90 - Neonatal outcomes in irreversible pulmonary dysplasia requiring extracorporeal membrane oxygenation: Experience from the Extracorporeal Life Support Organization Registry
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 90
Publication Number: 90.1733
Publication Number: 90.1733

Aditya S. Kalluri, MD, PhD (he/him/his)
Pediatrics Resident
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Irreversible pulmonary dysplasias (IPDs) are rare congenital malformations of the pulmonary parenchyma and vasculature such as alveolar capillary dysplasia and congenital acinar dysplasia; they often require neonatal extracorporeal membrane oxygenation (ECMO) and have poor survival. Older studies comparing outcomes in IPD to persistent pulmonary hypertension of the newborn (PPHN) found that IPD patients had later initiation of ECMO, longer treatment duration, and lower survival to discharge. Given new genetic insights for IPD and progress in medical management, we sought to characterize current outcomes for neonates with IPD and PPHN requiring ECMO using the Extracorporeal Life Support Organization (ELSO) database.
Objective: We hypothesized that newborns with IPD would have later initiation of ECMO, require longer total duration of therapy, and have lower survival to discharge, and that clinical advances would result in shorter ECMO duration and improved survival to discharge when comparing cohorts from 2011-2021 to 2000-2010.
Design/Methods: Data were obtained from the ELSO registry from 2000-2021 for neonates aged 0-28 days with ICD-9 and ICD-10 codes defining IPD and PPHN, excluding patients with diagnostic codes for congenital diaphragmatic hernia, meconium aspiration, pneumonia, or sepsis. Statistical comparisons were made using the Wilcoxon rank sum test for continuous variables or the Fisher’s exact test for categorical variables.
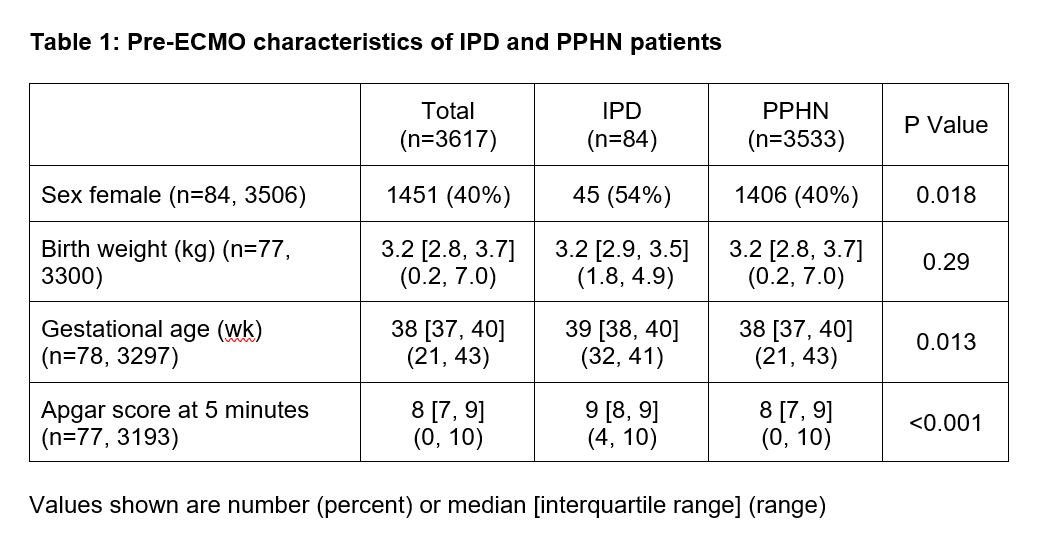
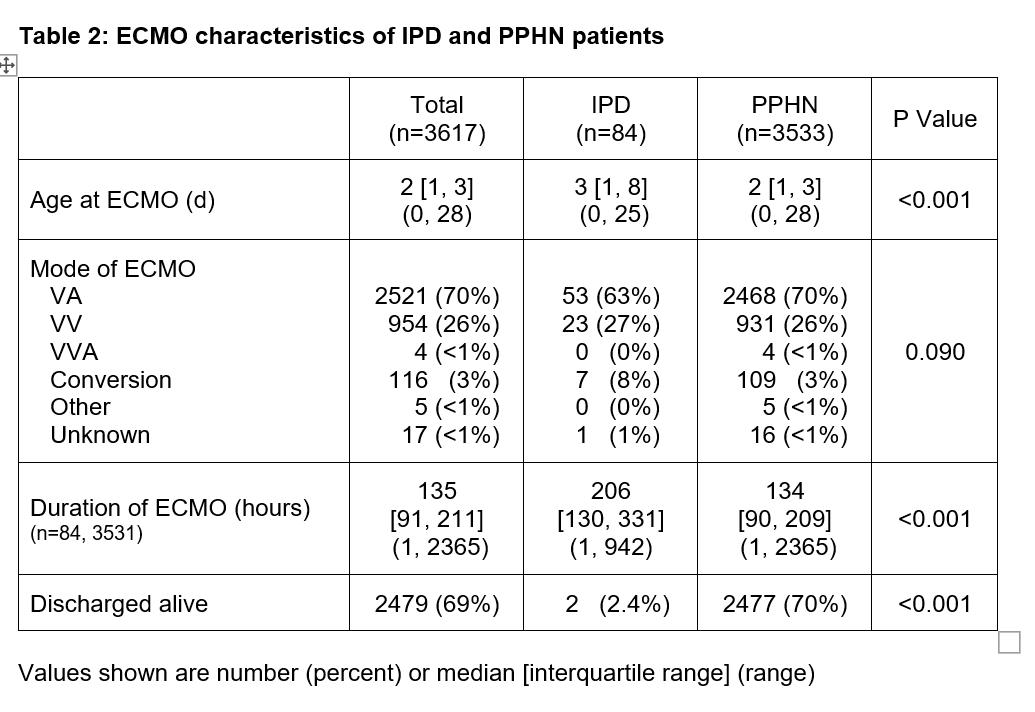
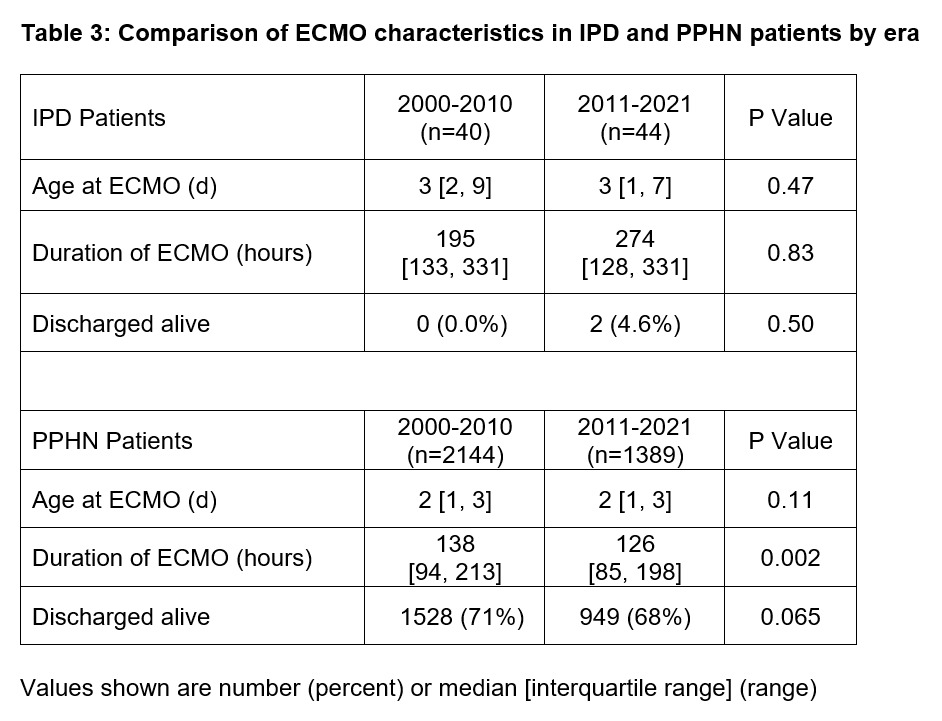
Results: There were 3,617 neonates aged 0-28 days requiring ECMO for IPD or PPHN; 84 were included in the IPD group and 3,533 in the PPHN group. Neonates with IPD were more likely to be female, had higher median gestational age by 1 week, and had a higher 5-minute Apgar score (Table 1). Those with IPD were older at the time of ECMO initiation by 1 day (Table 2). Patients with IPD also had a longer duration of ECMO (median 206 hours compared to 134 hours in the PPHN group). Patients with IPD had a significantly lower rate of survival to discharge than those with PPHN (2.4% vs 70%, P< 0.001). Comparison of the 2000-2010 and 2011-2021 periods showed no significant change in age at ECMO initiation or rate of survival to discharge in patients with IPD or PPHN.
Conclusion(s): Neonates with IPD requiring ECMO continue to require longer total duration of ECMO therapy and present with later ECMO initiation compared to those with PPHN. Despite clinical advances, duration of ECMO and survival to discharge for patients with IPD have not improved significantly in the last decade. Clinical and research innovations are needed for patients with these rare congenital disorders.