Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 9
325 - Identifying Barriers to Health Equity and Drivers for Improving Antibiotic Prescribing in Pediatric Urgent Care Settings
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 325
Publication Number: 325.1732
Publication Number: 325.1732

Rana E. El Feghaly, MD, MSCI (she/her/hers)
Professor
Children's Mercy Kansas City, UMKC
Kansas City, Missouri, United States
Presenting Author(s)
Background: Antibiotic prescribing differs by race, ethnicity, gender, age, socioeconomic demographics, and insurance in ambulatory settings. These differences likely represent structural inequities; however, little is known about the underlying drivers of these inequities, particularly in pediatric urgent care settings.
Objective: Identify causes of health inequities, and drivers and quality improvement (QI) tools for improving antibiotic prescribing practices by pediatric urgent care (PUC) clinicians through a multi-center national collaborative.
Design/Methods: We enrolled participants through a national QI collaborative whose goal is to improve health equities in antibiotic prescribing in PUCs. Each site identified clinicians and family representatives who participated in 4 focus group sessions to 1) define the problem of health inequity in antibiotic prescribing, 2) identify barriers to health equity, 3) delineate drivers to improved health equity, and 4) propose interventions that would be most impactful. Each focus group session was offered twice to accommodate schedules. The sessions were recorded and reviewed to identify themes regarding perceptions of health equity in antibiotic prescribing and the drivers of prescribing behaviors. We reviewed the sessions to assign codes and group them into broader categories.
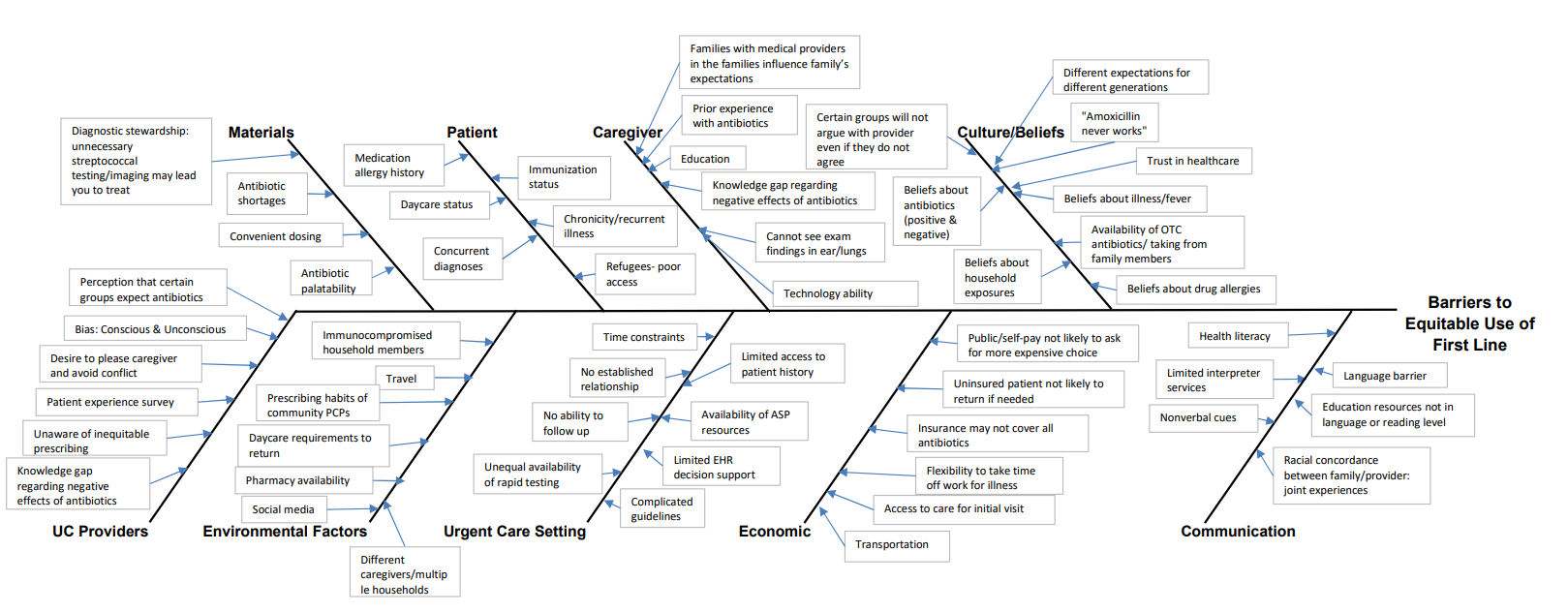
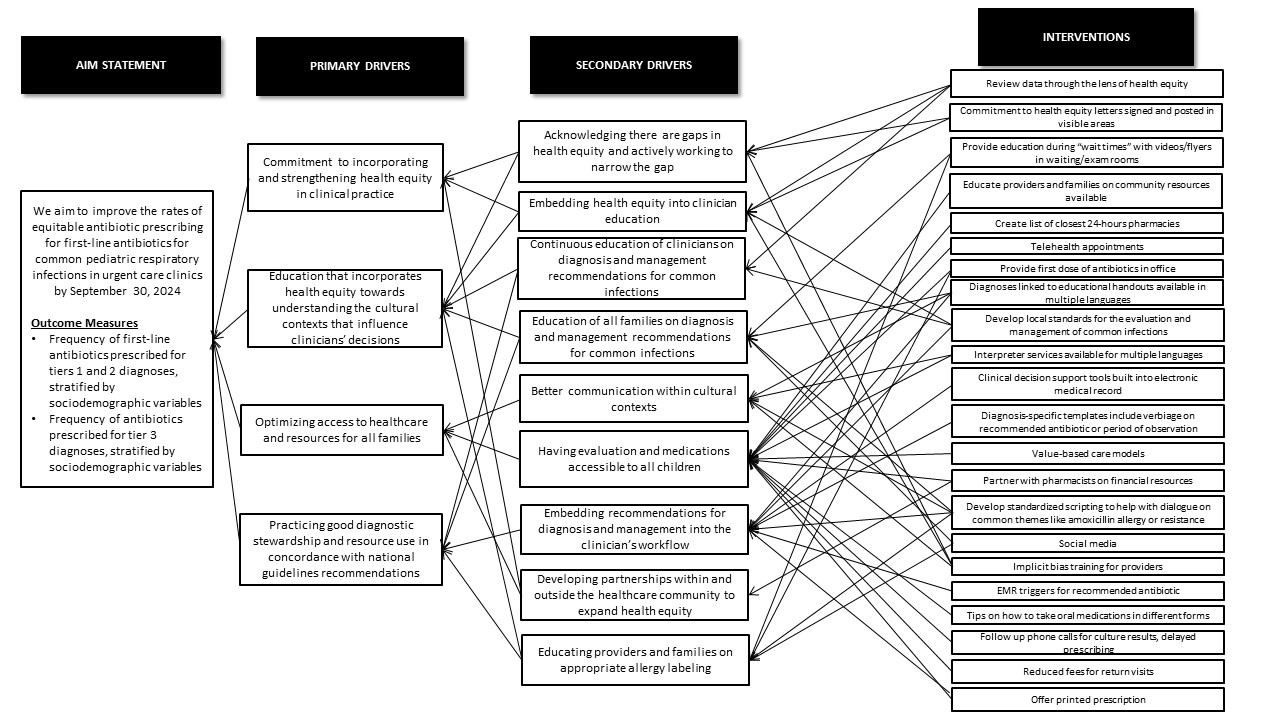
Results: A total of 31 sites from 22 states and Washington D.C. participated in the PUC collaborative. From April-August 2023, 131 individual participants (Table 1) completed our enrollment survey and attended the focus groups. Barriers to equitable prescribing included 9 domains (providers, caregiver, patient, urgent care setting, environmental factors, materials, cultural beliefs, economic, and communication) (Figure 1). Main drivers of improving prescribing included commitment to incorporating and strengthening health equity in clinical practice, education that incorporates heath equity, optimizing access to healthcare and resources, and implementing antibiotic and diagnostic stewardship practices in concordance with national guidelines. Multiple potential interventions impacting these drivers are listed in Figure 2.
Conclusion(s): Multiple studies have identified health inequities in antibiotic prescribing, however, barriers to health equity and drivers of improving prescribing have not yet been described. This national collaborative identified multiple potential drivers of improvement that will be used in a QI framework to improve health equities in antibiotic prescribing and decrease the prescribing gaps between the different patient populations.
.png)
