Neonatology
Session: Neonatal/Infant Resuscitation 1
255 - Supraglottic airway versus face mask for positive pressure ventilation in simulated neonatal resuscitation: a randomized cross-over trial
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 255
Publication Number: 255.3305
Publication Number: 255.3305
Victoria Blancha Eckels, MD (she/her/hers)
Assistant Professor of Pediatrics
Weill Cornell Medicine
Teaneck, New Jersey, United States
Presenting Author(s)
Background: Effective ventilation is the most critical step in neonatal resuscitation. Failure to provide adequate ventilation to neonates who are apneic or breathing insufficiently can lead to significant morbidity or mortality. Historically, positive pressure ventilation (PPV) is routinely administered with a face mask, which can be technically difficult and inadequate due to mask leak or obstruction. Providers responsible for initial PPV have varied training and experience levels. The supraglottic airway is an alternative device that can be used for PPV and may be easier to use and provide better ventilation during neonatal resuscitation.
Objective: To compare the supraglottic airway (SGA) to face mask (FM) for PPV during simulated neonatal resuscitation.
Design/Methods: In a randomized cross-over trial, neonatal airway provider and bedside nurse teams were randomized to complete a video-taped simulated neonatal resuscitation using the SGA or FM for PPV. The device (SGA or FM) was switched for a second simulated resuscitation by the teams. During PPV, inspiratory and expiratory tidal volumes were measured using a Respironics NM3 respiratory function monitor (Phillips, Andover, MA). The primary outcome was time to effective PPV (chest rise for at least five consecutive inflations). Secondary outcomes were number of inflations with chest rise, expired tidal volumes, leak, and device readjustments.
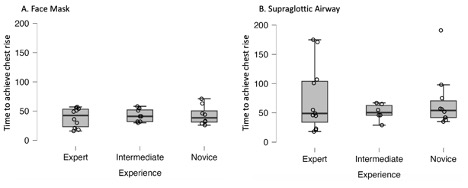
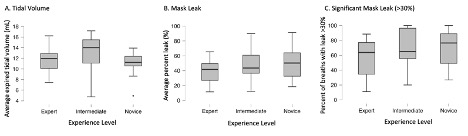
Results: Thirty teams completed a simulated resuscitation each with the SGA and FM (Table 1). Mean (SD) time to effective PPV was higher with SGA compared to FM (66.85 (46.21) vs. 41.23 (14.58) seconds; p=0.03) (Figure 1). Effective PPV was achieved from the first inflation in 15 (SGA) and 17 (FM) sessions. Three (SGA) and 4 (FM) teams never achieved effective PPV. There was no difference in percentage of inflations or longest run of inflations with chest rise. The mean (SD) number of readjustments was less with SGA than FM (0.60 (1.04) and 1.69 (1.2); p< 0.001). With the FM, mask leak, percent of inflations with leak >30%, and expired tidal volumes achieved were varied even among most experienced providers (Figure 2). The SGA mean (SD) leak was 60 (20.05) % and we discovered a misalignment in the manikin airway, therefore these data were excluded from our analysis.
Conclusion(s): Although effective PPV was achieved later with the SGA compared to FM, it was achieved from the first inflation equally with both devices. A similar number of teams never achieved effective PPV. Face mask PPV quality was variable across all providers. There remains a need to improve PPV during neonatal resuscitation and a potential role for the SGA.
.png)