Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 6
46 - Implementing Standardized Note Templates for Interns on Hospital Medicine Rotations
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 46
Publication Number: 46.3316
Publication Number: 46.3316

Benjamin Masserano, MD (he/him/his)
Pediatric Hospital Medicine Fellow
University of Texas Southwestern at Children's Health Dallas
Dallas, Texas, United States
Presenting Author(s)
Background: Resident physicians spend a significant amount of time on documentation within the electronic health record (EHR). This contributes to burnout, decreases face-to-face patient time, and creates extraneous information in the EHR.
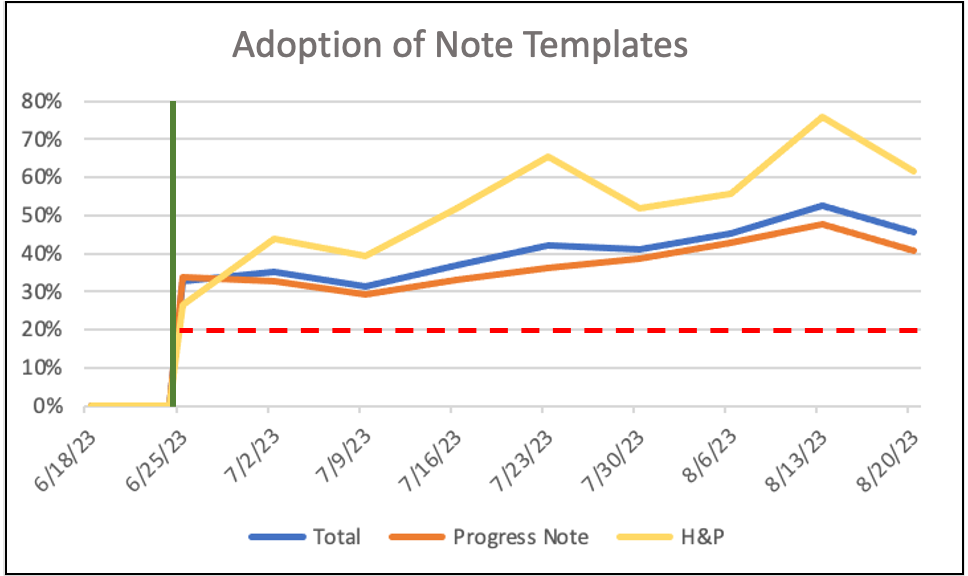
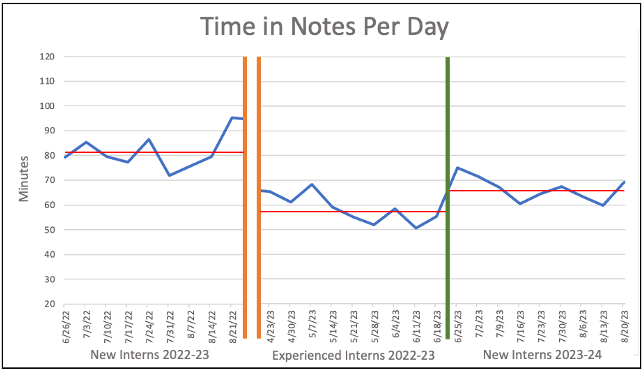
Objective: The primary aim of this quality improvement project was to reach 20% adherence to standardized note templates among interns rotating on the hospital medicine service. Secondary aims included reduction in note length and time spent in notes.
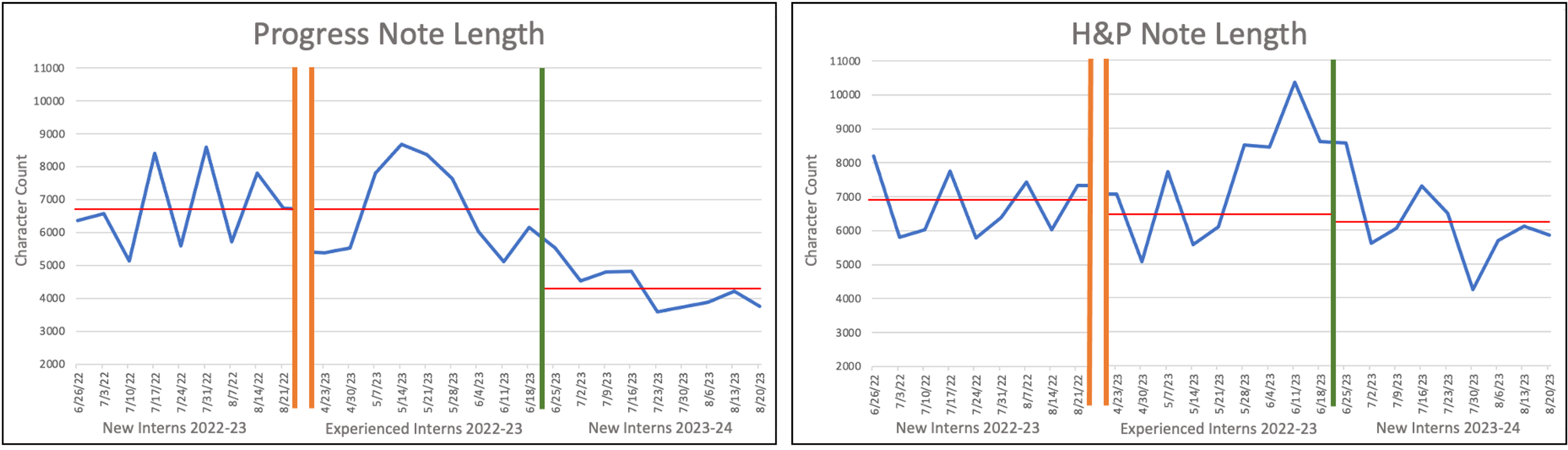
Design/Methods: This study utilized the EPIC (Verona, WI) EHR system. Note templates adhering to the 2023 inpatient billing requirements were created by a physician committee. These templates included embedded “help text” and EHR activity links to incorporate chart review into the note-writing workflow. Templates were introduced during the 2023 intern orientation, signage was posted on hospital computers, and residents and attendings were encouraged to use the templates via email. The study population included interns on hospital medicine rotations during the first 8 weeks of the academic year. Comparative pre-intervention data included interns on hospital medicine in the first and final 8 weeks of the previous academic year to account for clinical experience. Outcomes included adoption rates, note character counts, and time in notes per day.
Results: 38 interns rotated on hospital medicine services in the 8 weeks after our intervention with an average template adoption rate of 40.9%. During the study period there was a rise in template adoption. In the final week of data collection template adoption rates were 45.7% for all notes, 40.8% for progress notes, and 61.5% for history and physical notes. There was a 36.2% decrease in progress note length in characters between pre-intervention interns (new [6772], experienced [6749]) and post-intervention interns (4321) (p < 0.001). There was a 3.4% decrease in history and physical length in characters between experienced pre-intervention interns (6432) and post-intervention interns (6209) (p = 0.005). Time in notes per day decreased by 18.0% for post-intervention interns (66.5 minutes) as compared to new pre-intervention interns (81.2) (p < 0.001).
Conclusion(s): Implementation of standardized note templates with 40.9% adherence led to a significant decrease in note length and time in notes per day. Further research is needed to assess the effects of concise documentation on patient care and physician wellness.