Neonatology
Session: Neonatal Pulmonology - Clinical Science 4: Clinical Practice Questions, Going Home
557 - Skin to skin care reduces intermittent hypoxemia, stabilizing respiratory physiology in ventilated preterm infants
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 557
Publication Number: 557.3336
Publication Number: 557.3336
- AS
Arvind Sehgal, PhD (he/him/his)
MONASH UNIVERSITY
MELBOURNE, Victoria, Australia
Presenting Author(s)
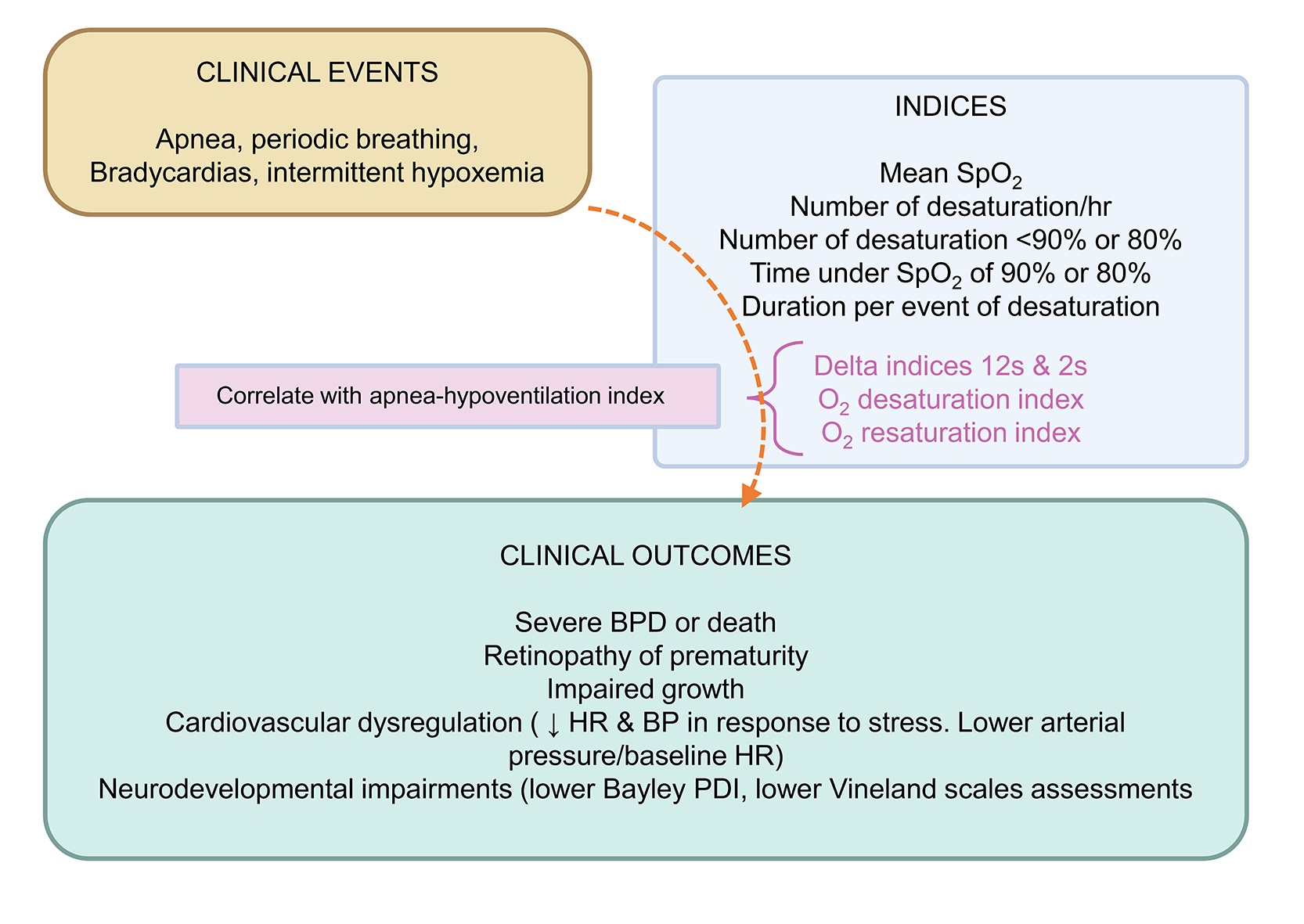
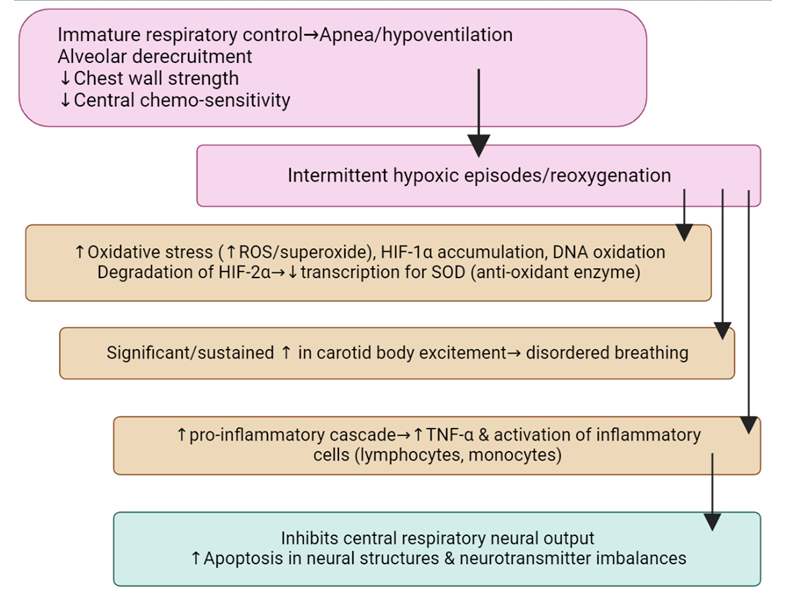
Background: Preterm infants are at risk of developing intermittent hypoxemia (IH), desaturations and bradycardia, which adversely influence clinical outcomes (Figure). The existing literature on the effects of skin to skin care (SSC) on preterm cardiorespiratory physiology is inconclusive.
Objective: To evaluate whether SSC in ventilated preterm infants improves indices of cardiorespiratory wellbeing.
Design/Methods: Continuous high-resolution pre-ductal pulse-oximetry recordings were performed using Masimo Radical-7® oximeter for one hour (incubator care [IC]) followed by one hour during SSC. Infants were ≤32 week’s gestational age (GA) at birth, 7-21 days of age, and managed on nasal CPAP; the pressure settings remained unchanged during the study. Each infant acted as its own control. Pulse oximetry was recorded at 2-second sample rate and 2-second averaging time. Definitions: (a) IH--> (i) Saturations (SpO2) < 90% and (ii) SpO2 < 85%, (b) Significant desaturations--> dips in SpO2 ≥4% and ≥5% from the baseline, (c) Bradycardia--> heart rate ≤80 beats/minute, (d) Delta index 12s--> sum of the absolute variations between two points in a 12 second period, divided by the number of 12s intervals (same calculation for 2s intervals, being the averaging time of the device), (e) Rapid resaturations--> increases of SpO2 of ≥3% within 10 second periods (f) Rapid desaturations--> decreases of ≥4% within 40 seconds. FiO2 is administered to maintain SpO2 within the nominated range (91-95%).
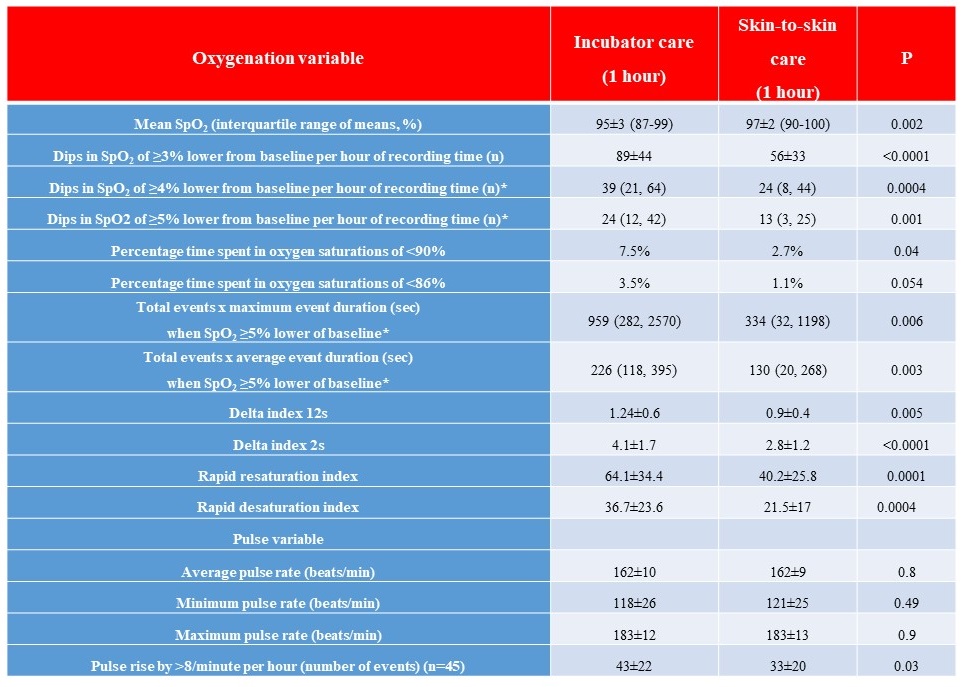
Results: The GA and birthweight of the 50 infants was 28.4±2.1 weeks and 1137±301g, respectively. Axillary temperatures (0C) and systolic BP before and at the end of SSC were comparable (36.8±0.2 [range, 36.2-37.2] vs 36.8±0.4 [range, 36-37.8], P=0.6) and (66±10 vs 65±11 mm Hg, P=0.8). Dips in SpO2 of ≥4% lower of baseline were significantly fewer with SSC, median (IQR) (39 [21, 64] vs 24 [8, 44], P=0.0004 and dips ≥5% lower of baseline, 24 [12, 42] vs 13 [3, 25], P=0.001, respectively. SpO2 variability (Delta 12 s and 2s), (1.24±0.6 vs 0.9±0.4, P=0.005 and 4.1±1.7 vs 2.8±1.2, P< 0.0001) and rapid resaturation & desaturation indices were significantly lower during SSC, compared to IC. Percentage time spent in oxygen SpO2 < 90% was lower with SSC (7.5% vs 2.7%, P=0.04). Mean heart rate was comparable although fluctuations in heart rate (rise by >8 beats/min) were lower with SSC (43±22 vs 33±20, P=0.03). Seven (14%) infants had bradycardias during IC and none during SSC, P=0.012) (Table, Figure).
Conclusion(s): SSC improves cardiorespiratory stability and reduces IH. Regular SSC for preterm infants has the potential to improve clinical outcomes.