Neonatology
Session: Neonatal General 4: Nutrition, Feeding, and Growth
92 - Does maternal microbiome impact growth parameters in preterm infants?
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 92
Publication Number: 92.604
Publication Number: 92.604

Swetha Padiyar, MD FAAP C-NNIC (she/her/hers)
Assistant Professor
Cleveland Clinic Children's Hospital
Westlake, Ohio, United States
Presenting Author(s)
Background: Globally, each year, over 13 million infants are born prematurely with about 10% of them delivered between 28-32 weeks. Prematurity contributes to one million neonatal deaths yearly, and the surviving infants are predisposed to cardiorespiratory, neurodevelopmental, and growth abnormalities with long-lasting sequelae. Preterm infants have significantly different microbiome than their term born peers. It is unclear if preterm birth causes attenuation of the establishment of the normal microbiome. The influence of maternal microbiome on fetal growth and development during pregnancy and infant’s microbiome in the postnatal period has been poorly understood.
Objective: The purpose of this study is to understand the influence of maternal microbiome on infant’s microbiome and birth anthropometry.
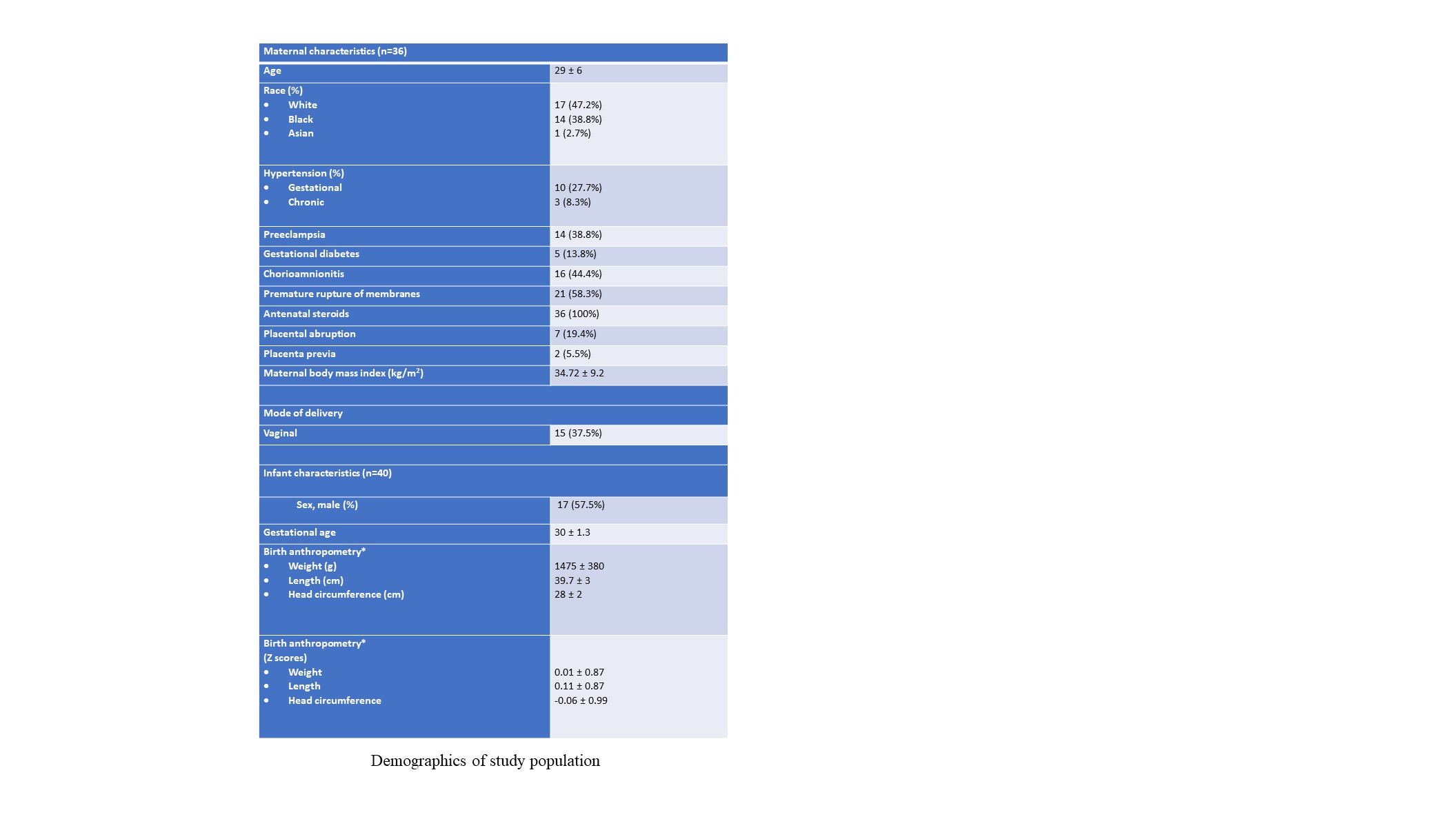
Design/Methods: This is a prospective cohort study that included infants born between 28-32 weeks of gestation and their mothers. Informed consent was obtained for all mother-infant dyads. Maternal rectal and vaginal samples and infant stool samples were collected at the time of delivery. Total bacterial community was amplified using PCR of the marker gene for 16s rRNA. 16s rRNA gene amplification was analyzed using Divisive Amplicon Denoising Algorithm (DADA2) pipeline. Linear regression models in R with bacteria quantity and other continuous variables, were transformed to meet model assumptions. ComBat was used for batch correction. White’s non- parametric t-test, ANOVA post hoc analysis were performed.
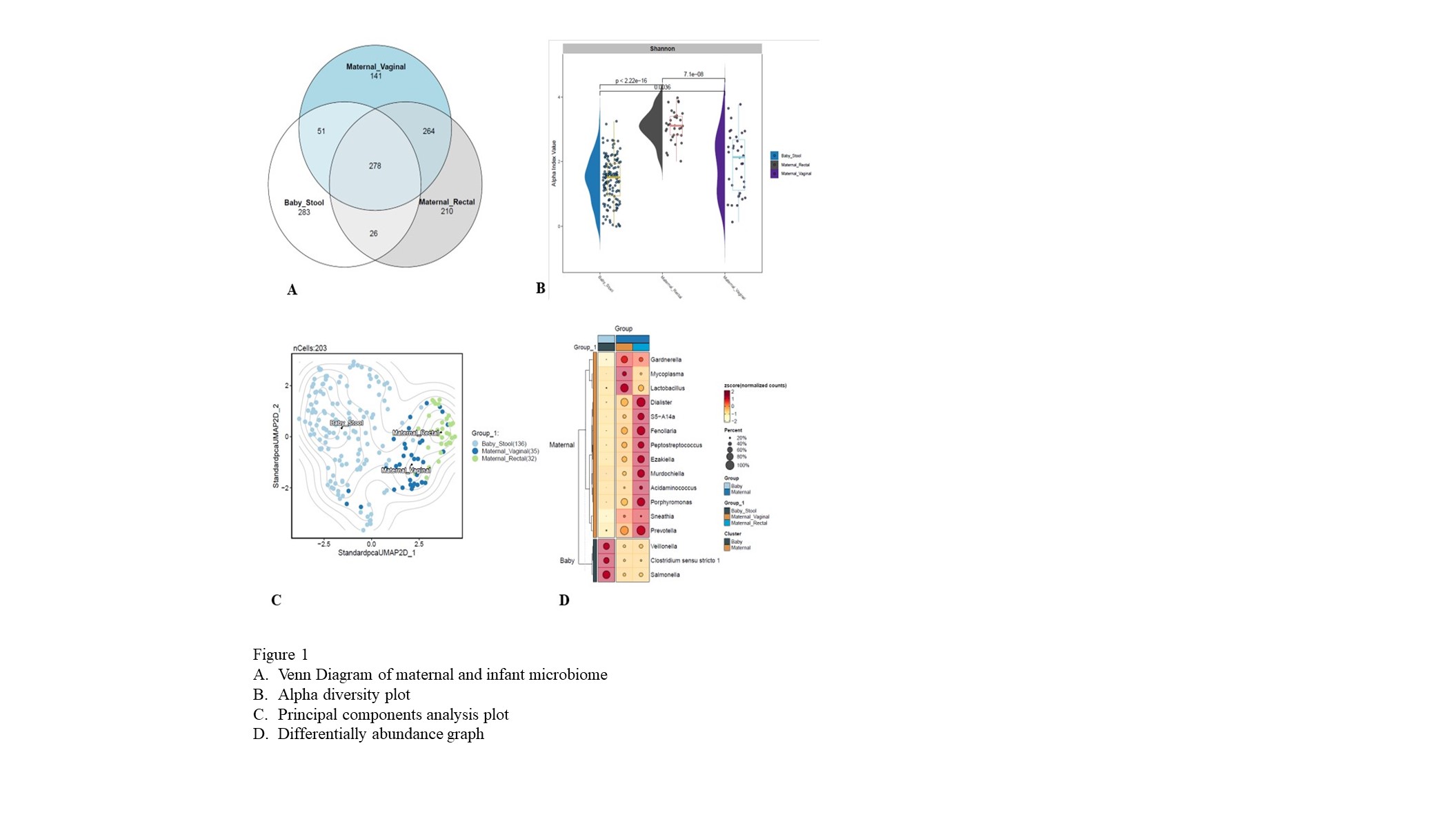
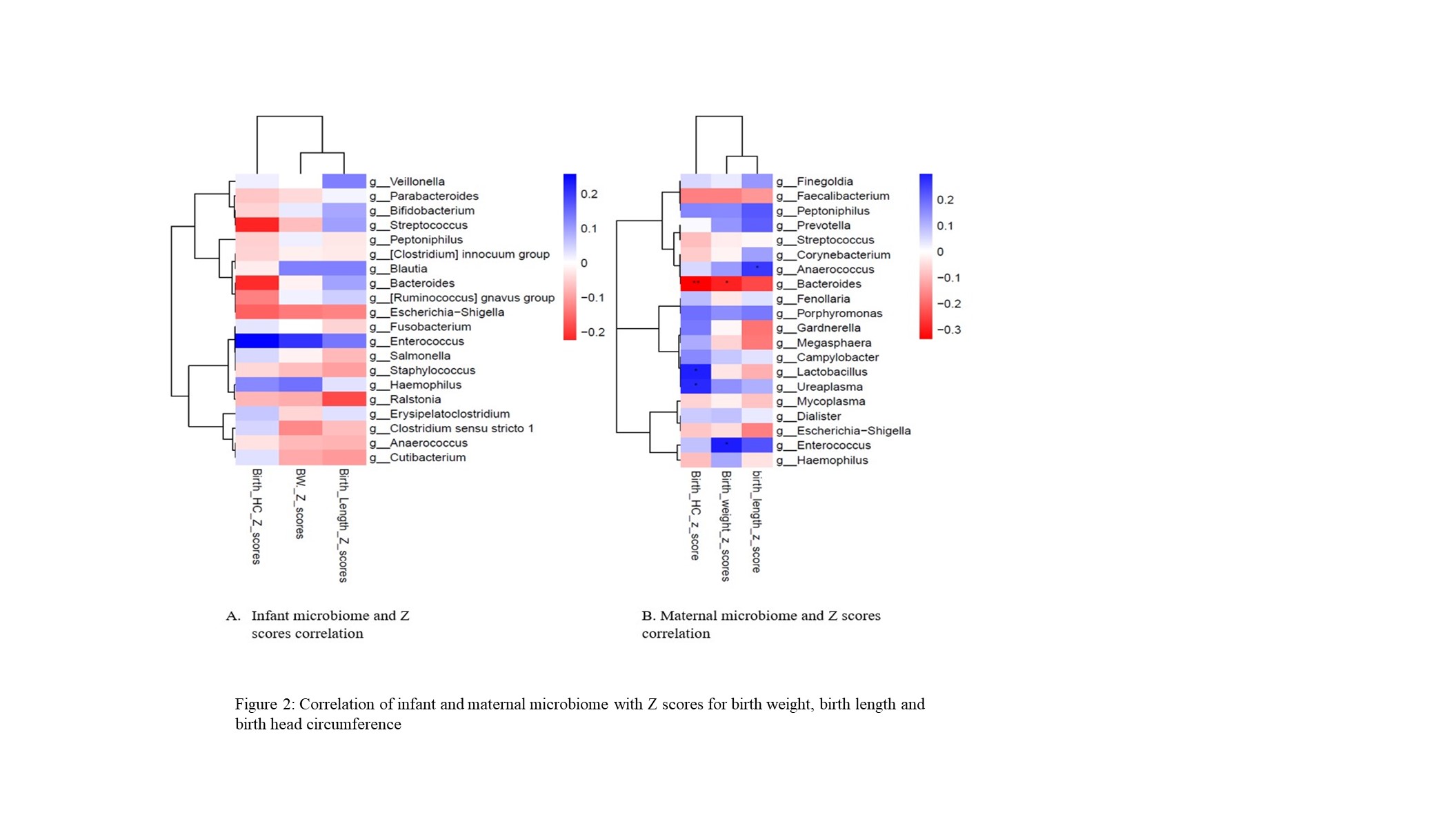
Results: 40 mother-infant dyads- 36 singleton and 4 twin gestation (Table 1.) Vaginal microbiome had a greater overlap with infant’s microbiome compared to rectal microbiome (51 vs 26). The microbiome α diversity was significant between all samples (p < 0.05) (Figure 1.). Maternal vaginal samples were high in Lactobacillus and Enterococcus. Maternal rectal samples were abundant in Finegoldia and Prevotella. Infant samples were high in Salmonella, Enterococcus and Staphylococcus. Infants born via C section had higher Staphylococcus counts whereas vaginally delivered infants had higher Streptococcus. Significance was observed between infant’s birth length and vaginal microbiome (p=0.0361) (Figure 2.). Post-hoc analysis at 95% confidence interval was significant for Staphylococcus, Salmonella and Prevotella (p < 0.001).
Conclusion(s): Salmonella is the predominant microbiome in preterm infants. Maternal and infant microbiome influences birth anthropometry. Maternal vaginal microbiome influences infant’s microbiome but may not be the only source of infant’s microbiome.