Neonatology
Session: Neonatal General 4: Nutrition, Feeding, and Growth
101 - Rate of Metabolic Bone Disease of Prematurity: Incidence in a Single Center
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 101
Publication Number: 101.209
Publication Number: 101.209

Shayla Percy, MD
Neonatal-Perinatal Fellow
Children's Hospital of Pittsburgh
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Background: Metabolic bone disease of prematurity (MBDP) refers to the reduction in bone mineral content of infants born prematurely when compared to term infants and is associated with radiographic and biochemical changes. Infants born prior to 29 weeks gestation are at highest risk as 66-80% of all fetal phosphorus and calcium accretion occurs during the third trimester of pregnancy. MBDP has a wide reported incidence of 20-60% of premature infants – likely because there is no universal definition. The incidence of fractures is also widely variable, from 10-43% of patients with MBDP.
Objective: The aim of this project was to analyze the baseline rate of MBDP and incidentally found fractures at University of Pittsburgh Medical Center’s (UPMC) level III and IV neonatal intensive care units.
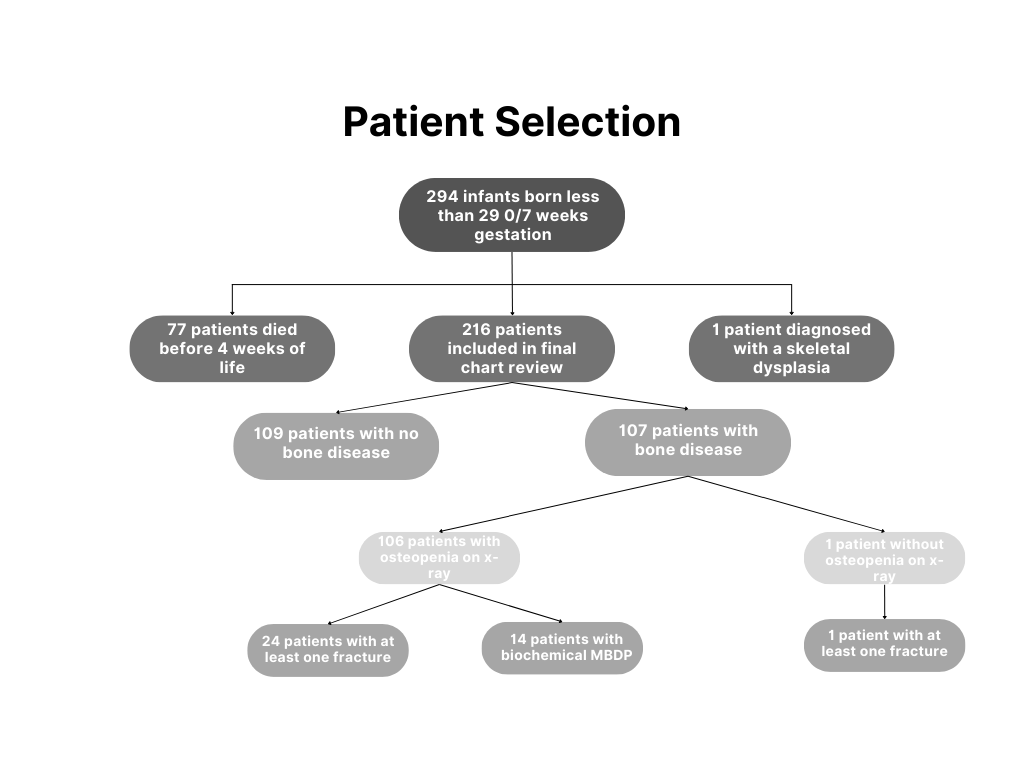
Design/Methods: Data was collected as part of an ongoing quality improvement initiative. A manual chart review was performed on all infants born less than 29 0/7 weeks gestation who were in-born or transferred to UPMC within one week of life for demographics, presence of fractures or osteopenia on x-ray, diagnosis of biochemical MBDP (alkaline phosphatase >600 IU/L and phosphorus < 4.5 mg/dL over two consecutive checks), medications administered, and method of feeding.
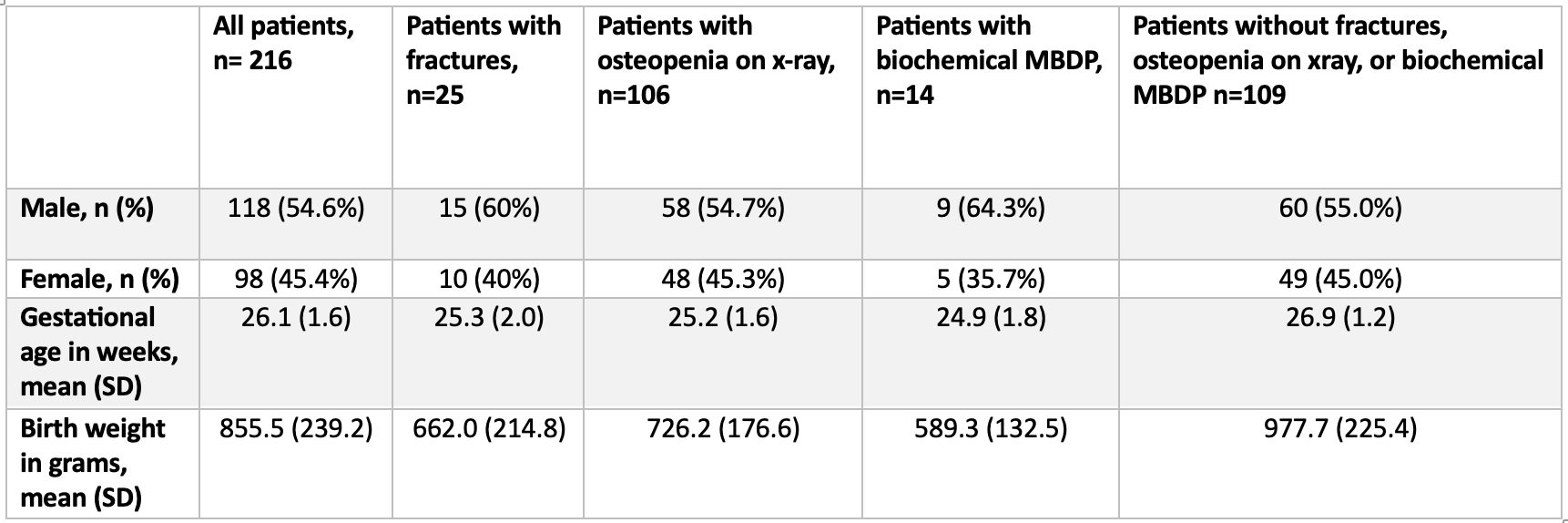
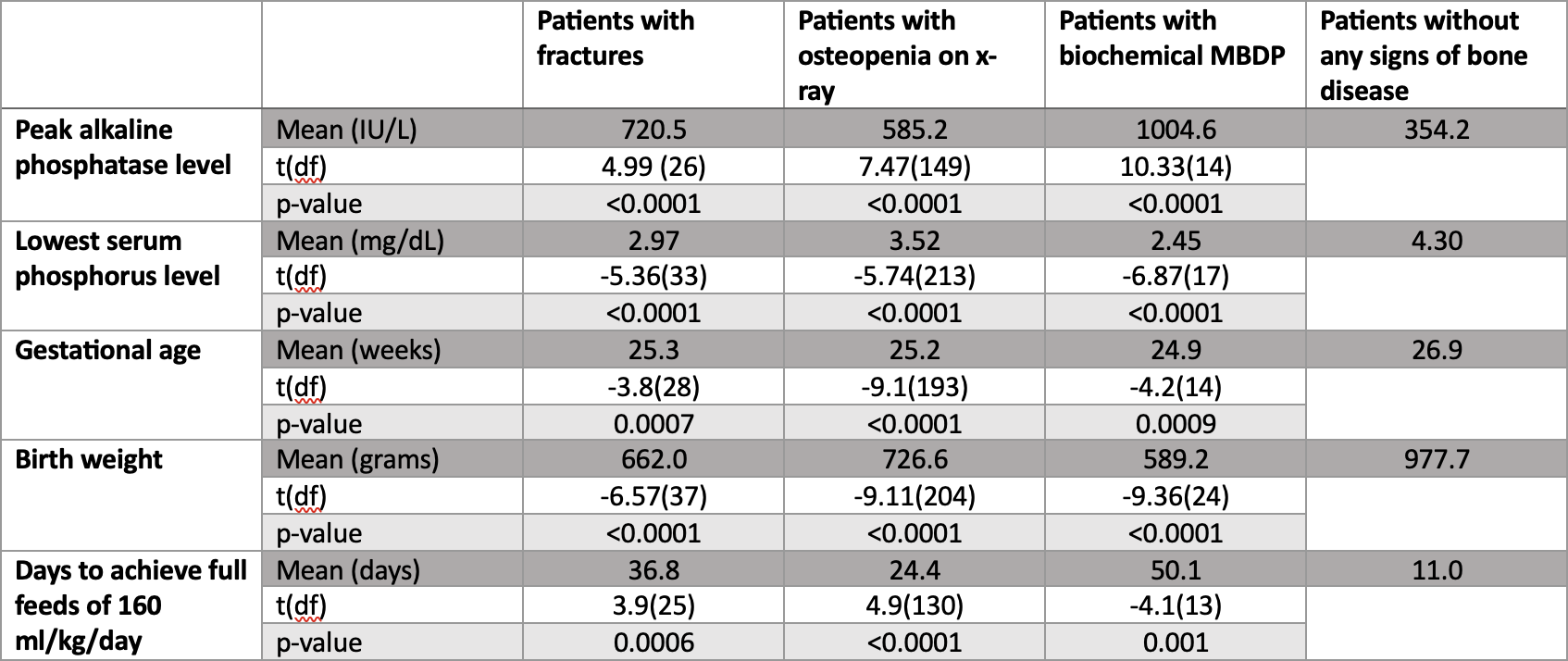
Results: A total of 294 patients met criteria for review between June 2021 and June 2023. 78 patients were excluded secondary to skeletal dysplasia or death prior to four weeks of age. 216 patients were included in the final chart review (Figure 1, Table 1). Of these patients, 11.6% (n=25) had at least one incidentally found fracture and 49.1% (n=106) had evidence of osteopenia on x-ray. Biochemical MBDP was found in 6.5% (n=14) of infants and denoted a PPV of 100% for osteopenia on x-ray and 92.9% for fracture. Infants who presented with a fracture, osteopenia on x-ray, and/or biochemical MBDP had significantly lower birth weights, lower gestational ages, longer duration to achieve full feeds, higher peak alkaline phosphatase levels, and lower nadir phosphorus levels (Table 2). Finally, calcium and/or phosphorus supplementation – the mainstay of treatment for MBDP – did not occur in 36% (n=9) of the patients with reported fractures.
Conclusion(s): This single center review found an incidence consistent with the previously reported rates in the literature and reinforced the significance of previously known risk factors. This review also indicated a need for clinical change in mineral supplementation and feeding advancement in this center. Additional studies and improvement initiatives are required to work towards improving the bone health of premature infants.