Emergency Medicine
Session: Emergency Medicine 4: Infections
111 - Testing and Treatment Thresholds for Community-Acquired Pneumonia in the Pediatric Emergency Department
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 111
Publication Number: 111.1368
Publication Number: 111.1368

James Rudloff, MD (he/him/his)
Clinical Fellow
Washington University in St. Louis School of Medicine
Saint Louis, Missouri, United States
Presenting Author(s)
Background: Clinical prediction tools can improve the diagnosis of community-acquired pneumonia (CAP) in the emergency department (ED), though their use is not widespread. A better understanding of clinician testing and treatment thresholds for CAP may facilitate implementation of clinical prediction tools to improve care.
Objective: To elucidate thresholds for chest radiograph (CXR) performance and empiric antibiotic treatment in the absence of CXR for CAP among children presenting to the ED with respiratory illness.
Design/Methods: We performed a cross-sectional survey of emergency medicine clinicians in the AAP Section on Emergency Medicine. Clinicians were presented with 8 clinical vignettes for hypothetical patients aged 5 months to 18 years with respiratory symptoms. They were asked to state their suspected likelihood of CAP and to choose whether they would obtain a CXR or give empiric antibiotics. Clinicians were then provided the estimated probability of radiographic CAP based on a validated prediction tool designed for children with suspected CAP and were re-surveyed. Logistic regression was used to determine the thresholds for testing and treatment, which were defined as the disease probability in which half of clinicians would test and treat, respectively.
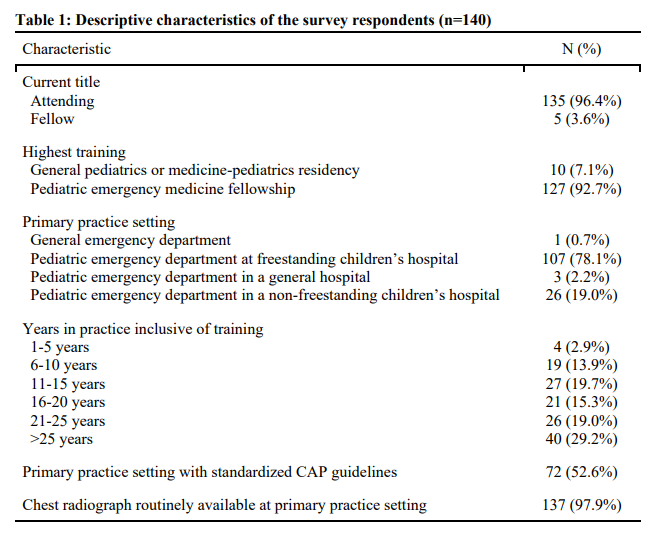
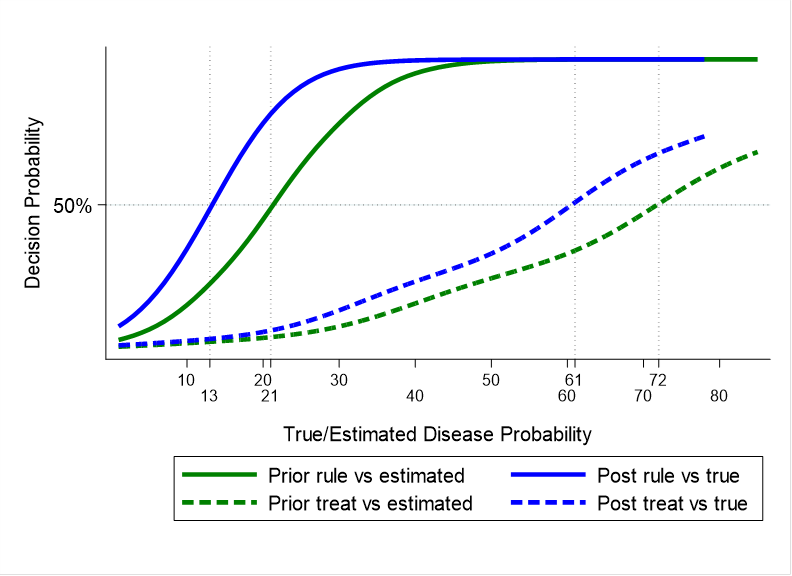
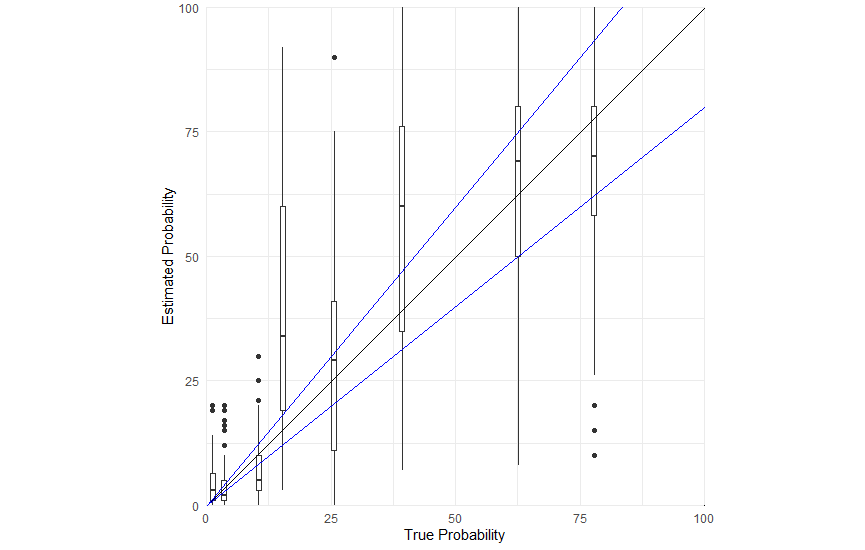
Results: One-hundred forty (29.4%) of 476 eligible respondents completed the survey. Most respondents were attendings (96.4%), completed a pediatric emergency medicine fellowship (92.7%), and were practicing in a freestanding children’s hospital (78.1%, Table 1). Half (52.6%) of clinicians practice in settings with institutional guidelines for CAP and nearly all (97.9%) have CXR readily available. For six of the eight vignettes, there were statistically significant differences between clinicians’ estimated probability and the “true” probability from the validated prediction tool (Figure 1). Testing and treatment thresholds for CAP were 21% and 72%, respectively, prior to knowledge of the tool-based probability (Figure 2). When provided the estimated probability of CAP based on a validated clinical prediction tool, testing and treatment thresholds were 13% and 61%.
Conclusion(s): Compared to a validated prediction model, physicians lacked accuracy when estimating CAP and had wide variability of test and treat thresholds across most clinical scenarios/vignettes. Knowledge of these thresholds could inform implementation of clinical decision tools including defining a clinical threshold for “low-risk” patients that would not benefit from a chest x-ray or empiric antibiotics.