Neonatology
Session: Neonatal/Infant Resuscitation 2
280 - Factors that affect the umbilical vessel closure in an asphyxiated preterm ovine model
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 280
Publication Number: 280.2995
Publication Number: 280.2995

Mausma Bawa, MD (she/her/hers)
Resident Physician
Boston Children's Hospital
Brookline, Massachusetts, United States
Presenting Author(s)
Background: Delaying the clamping of the cord is beneficial in preterm newborns. Roach et al. (1971) studied the effect of muscle coiling when there was a drop in temperature to 25 C. Meyer et al. (Eur. J. Ped 1978) studied the structural effect of umbilical artery mechanical closure. Other than placental separation/mechanical closure, it is unclear if factors such as neonatal/maternal heart rate (HR), blood gas parameters, and neonatal hemodynamics can influence umbilical blood flows.
Objective: Our objective was to evaluate the factors that affect umbilical vessel closure in an asphyxiated preterm ovine model.
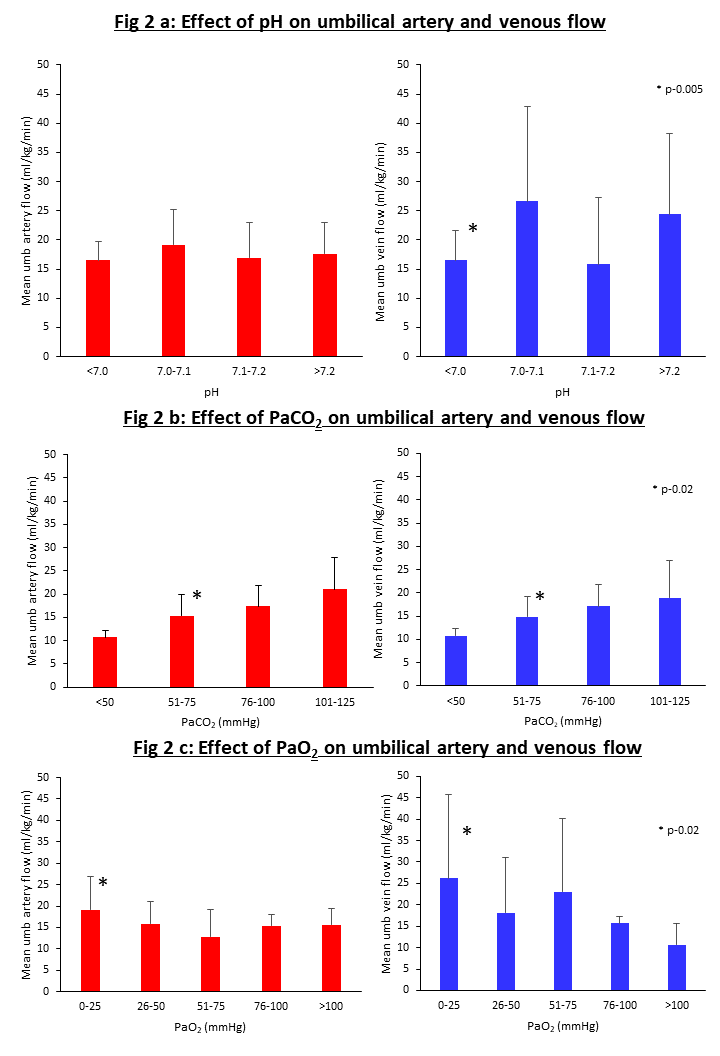
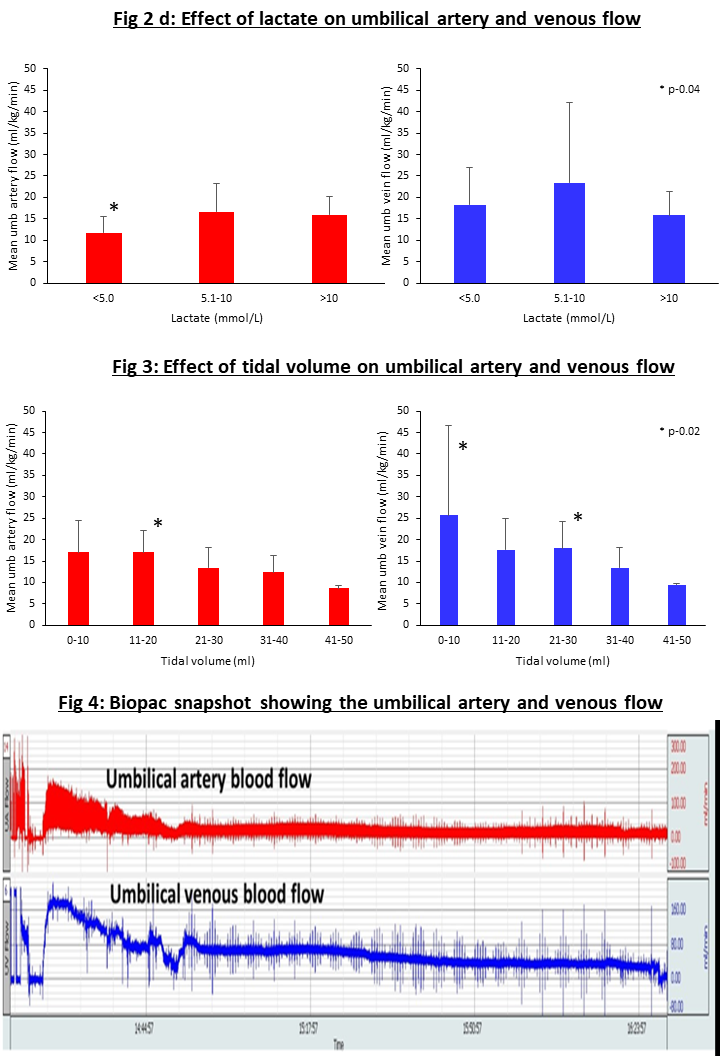
Design/Methods: We used time-dated pregnant ewes of 126-128 days gestational age (~28wk human neonates) as per ARRIVE guidelines after approval by IACUC. The lamb was instrumented while in placental circulation; with the ewe under general anesthesia. Asphyxia was induced by umbilical cord occlusion to achieve heart rate (HR) < 90bpm. Lambs were ventilated with intact cord for 2 hours using supplemental oxygen per neonatal resuscitation guidelines and tidal volume (TV) of 8-10 ml/kg. Data on umbilical venous (UV) and umbilical arterial (UA) flow, maternal (ewe) and neonatal (lamb) HR, gas exchange including pH, arterial carbon dioxide (PaCO2), arterial oxygen (PaO2) and lactate was recorded for 2 hours post resuscitation. We further delineated each of the parameters to different groups to evaluate the effect on umbilical vein and artery flows as shown in the figures.
Results: A total of 10 preterm lambs were used in our study. We excluded 3 lambs due to arrhythmia. There was no difference on UV or UA flows with varying maternal HR (Fig 1a). The UA flow was significantly different with varying neonatal HR. The UV flow was not different between different neonatal HR (Fig 1b). There was no difference in UA flows with pH. The UV flow was significantly different with varying pH (Fig 2a). There was a significant difference in both UA and UV flows with a change in PaCO2 (Fig 2b). The UA flow was significantly different with lower PaO2 (Fig 2c). The UA flow significantly differed with a lactate change (Fig 2d). We also noted significant changes in both UA and UV flows with changes in tidal volume (Fig 3).
Conclusion(s): Our study in preterm asphyxiated lambs shows that pH, arterial carbon dioxide levels, hypoxemia, and lactate levels could affect the umbilical flows. These factors may play a role in physiological umbilical cord closure and the localized contractions following cord clamping. More studies are needed to understand the closure to help determine the clamping of the cord for optimal benefit.
.png)