Neonatology
Session: Neonatal General 2: NICU Care Strategies
71 - Neonates with Critical Congenital Heart Disease and Growth Failure
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 71
Publication Number: 71.385
Publication Number: 71.385
.jpg)
Joanne Newens, BS (she/her/hers)
Medical Student
University of California, Los Angeles David Geffen School of Medicine
Los Angeles, California, United States
Presenting Author(s)
Background: Neonates with critical congenital heart disease (CHD) require prolonged hospital stays secondary to multiple surgeries and high rates of sepsis and necrotizing enterocolitis. These complications combined with suboptimal nutrition lead to growth failure (GF) and have far-reaching consequences including neurodevelopmental delays.
Objective: This retrospective, single-site study aimed to investigate the early incidence of GF and characterize GF in hospitalized infants with cCHD.
Design/Methods: Inclusion criteria included neonates with cCHD requiring neonatal intensive care, a postnatal echocardiogram confirming cCHD (transposition of the great arteries, truncus arteriosus, hypoplastic left heart syndrome, single left ventricle, double inlet left ventricle, double outlet right ventricle, pulmonary atresia with intact pulmonary septum, Ebstein’s anomaly, atrioventricular canal, Tetralogy of Fallot, total and partial anomalous pulmonary venous return, Shone’s complex, coarctation of aorta) and baseline anthropometric measurements. Weight and length z-scores were collected at birth and approximately 14, 21, and 30 days of age, and discharge. The primary outcome of the study was growth failure at discharge, defined by weight and length z-score changes and further characterized by severity (none; mild, z-score decline of 0.8-1.2; moderate, decline >1.2-2; severe, decline ≥ 2).
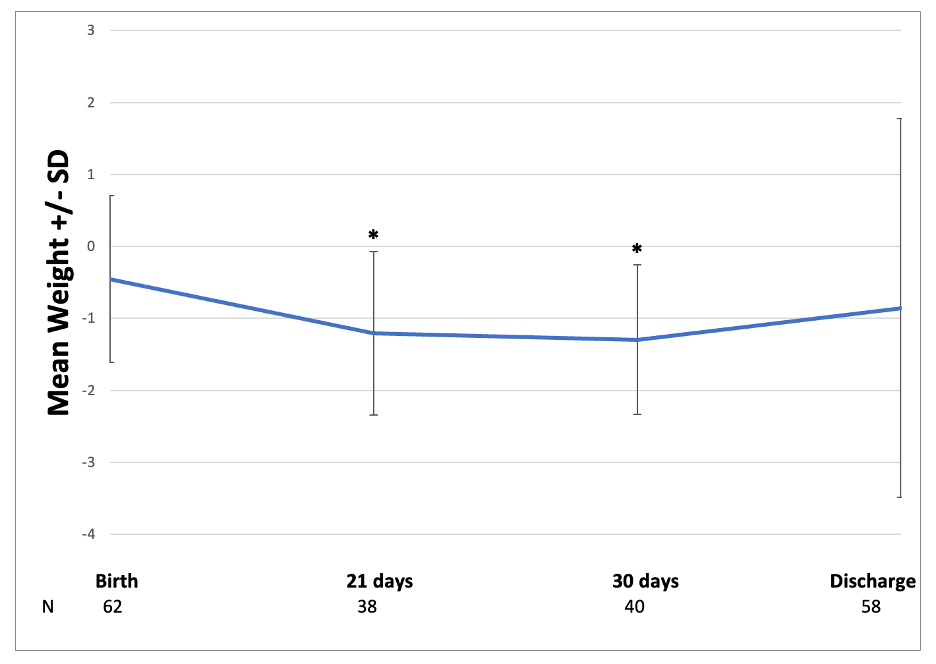
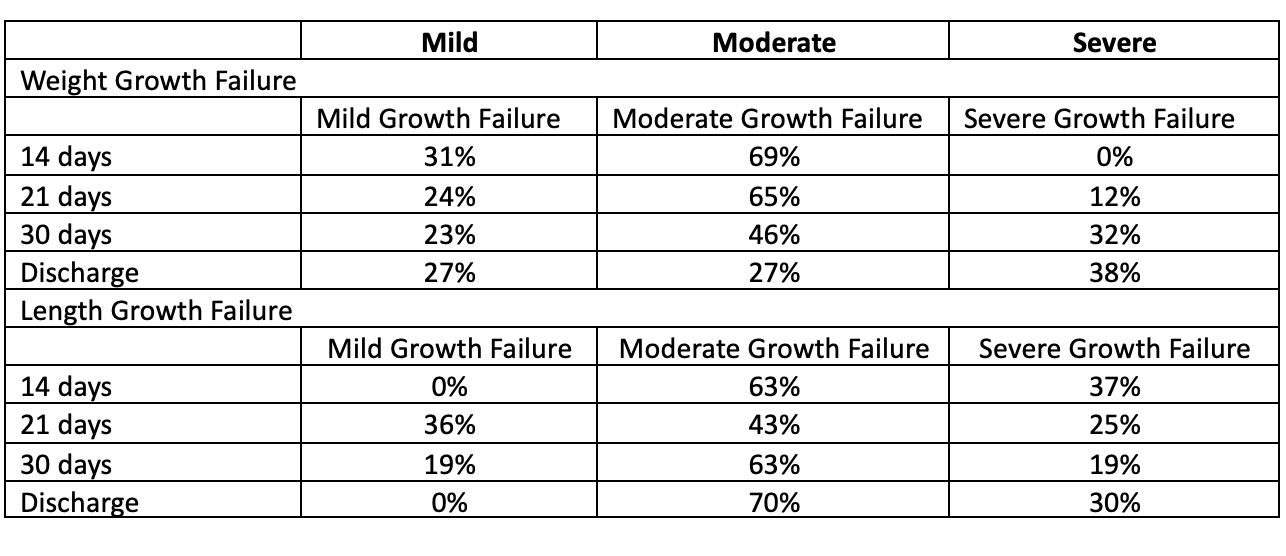
Results: The mean (SD) gestational age was 38.1 (2) weeks, length of stay was 31.5 (59) days, and birth weight is 3.1 (0.6) kg. When compared to birth weight z-scores, weight z-scores at 21 days (-0.5 (1.2) vs. -1.2 (1.1), p< 0.01) and 30 days (-0.3 (1) vs -1.3 (1), p< 0.01) were significantly less (Figure). A similar trend was noted for length. When compared to birth length z-scores, length z-scores at 21 days (0.1 (1.4) vs. -0.62 (1.5), p< 0.05) and 30 days (0.1 (1.1) vs -0.9 (1.2), p< 0.01) were significantly less. The severity of GF increased over time (Table).
Conclusion(s): In this study, weight and linear GF was common in neonates with cCHD and increasing rates of GF occurred during the neonatal hospitalization. This data suggests that nutritional support may be inadequate. It remains unclear how GF alters neurodevelopment in infants with cCHD.