Mental Health
Session: Mental Health 2
572 - Implementing Suicide and Depression Screening in Acute Care Settings of a Pediatric Hospital System
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 572
Publication Number: 572.2257
Publication Number: 572.2257

Nicole Penwill, MD, MPH (she/her/hers)
Assistant Professor, Section of Hospital Medicine
Children's Hospital Colorado
Denver, Colorado, United States
Presenting Author(s)
Background: Suicide is the 2nd leading cause of death in youth ages 10-18, and over 40% of decedents are evaluated in a healthcare setting in the 30 days prior. There is a critical need to enact universal youth suicide and depression screening across healthcare settings.
Objective: Implement synchronous depression and suicide screening for patients 10 years and older in the emergency departments (EDs) and inpatient settings of a pediatric hospital system.
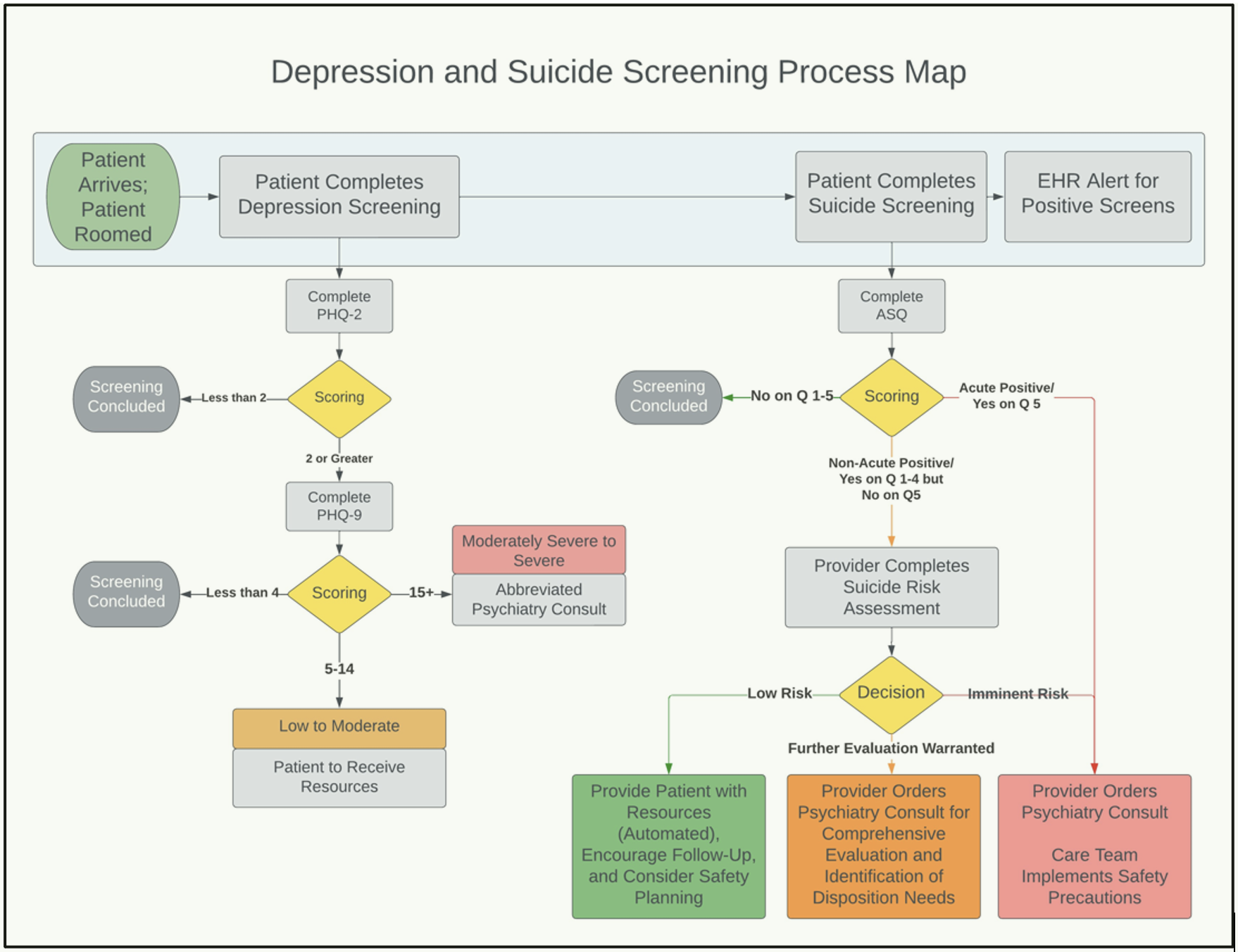
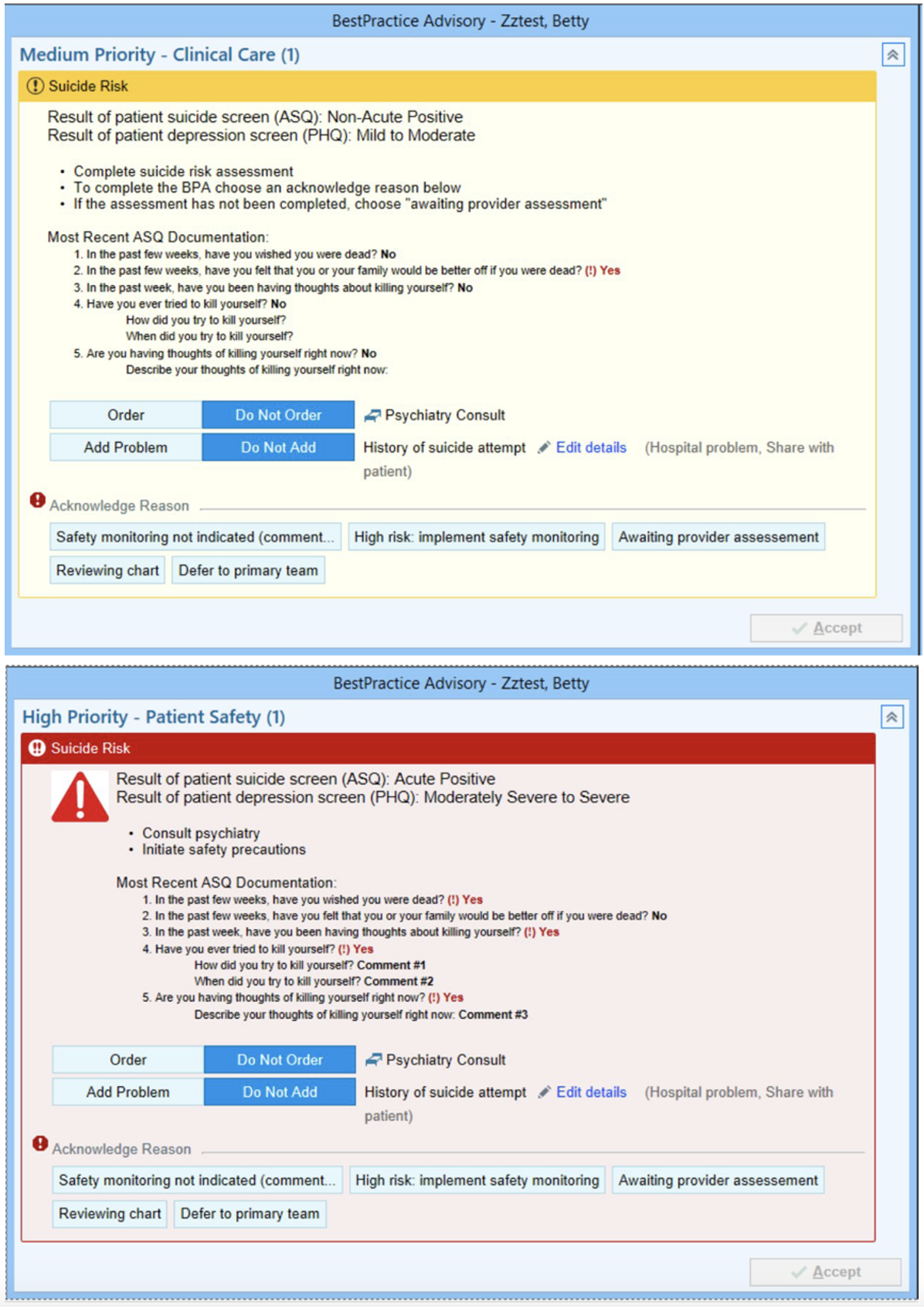
Design/Methods: A multidisciplinary team applied Design for Six Sigma methodology to characterize current state, design project elements, and strategize implementation. Prioritized design elements included use of validated screeners (modeled after the NIH Suicide Risk Screening Pathway), electronic heath record (EHR) integration, and synchronous depression and suicide screening workflows. Multiple venues/modalities were utilized to educate frontline clinicians and solicit input. Primary outcome measures were depression and suicide screening rates for patients in ED/inpatient units. Balancing measures included ED length of stay (LOS), 1:1 attendant orders, and psychiatry consults. We piloted screening in 2 EDs and 2 inpatient units across 2 hospital campuses prior to broader system-wide implementation.
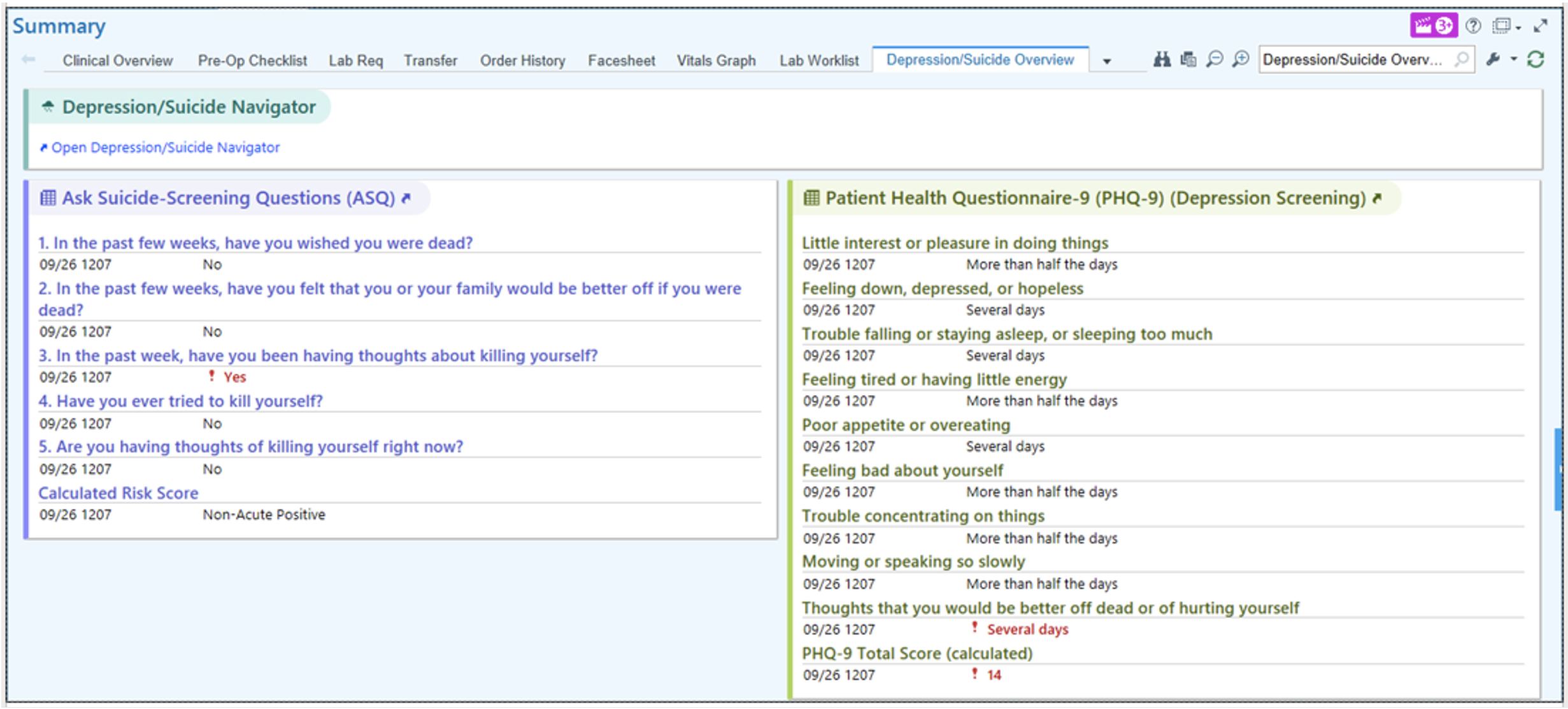
Results: We utilized three validated screening tools: Patient Health Questionnaire (PHQ)-2/9, Ask-Suicide-Screening-Questions (ASQ), and the Brief Suicide Safety Assessment (BSSA). Nurses administer the ASQ and PHQ-2/9, triggering EHR-clinical decision support, which directs further risk assessment by providers if indicated (BSSA piloted in select units), psychiatry consultation, and/or initiation of safety precautions (Figure 1). A “Depression and Suicide Navigator” page serves as the central EHR hub for screening results, safety planning, and documentation. An EHR-based depression/suicide data dashboard tracks outcome, process, and quality measures. Five months after implementation, we achieved depression and suicide screening rates of 80.9% and 85.6%, respectively. ED LOS, 1:1 attendant use, and psychiatry consults (per 1000 patient encounters) did not increase.
Conclusion(s): We operationalized universal depression/suicide screening in 2 EDs and 2 inpatient units of a pediatric hospital system. Our process centered on robust EHR-integration including of screening results, follow-up assessments, safety planning, and written educational materials. Future work includes expansion to ambulatory settings and system-wide rollout of the BSSA. This work may be generalizable to other hospitals planning to enact depression/suicide screening in ED/inpatient settings.