Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 5
41 - Lead Screening in the Pediatric Primary Care Setting: A Quality Improvement Initiative
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 41
Publication Number: 41.2931
Publication Number: 41.2931
Sarah A. Frantz, MD (she/her/hers)
Pediatrics Resident
NewYork-Presbyterian Morgan Stanley Children's Hospital
New York, New York, United States
Presenting Author(s)
Background: Lead risk assessment is recommended by the American Academy of Pediatrics at well child visits from 6 months to 6 years. Children at this age are at risk of elevated lead due to hand-to-mouth behaviors, increased absorption from their GI tracts, and less developed blood-brain barriers. Lead causes serious effects even at low levels including learning and behavioral issues. Blood lead testing is recommended if risk assessment questions indicate potential exposure to lead such as peeling or damaged paint, painted toys, spices/food/pottery from other countries, etc. At our urban academic practice we universally test for lead at 1 and 2 years of age based on New York City Department of Health recommendations. We universally test at 3 years of age given our high-risk population, and we test those aged 4-6 years who have developmental delays with mouthing behaviors.
Objective: This resident-led, QI project aimed to increase appropriate lead testing rates from a baseline median rate of 83% to a goal of 90% between October 2022 and May 2023.
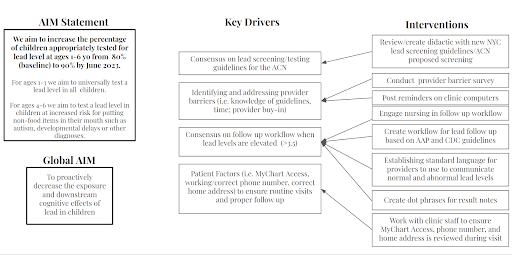
Design/Methods: A collaborative team of residents, faculty, nurses, and administrators met to identify the current lead screening guidelines, existing workflow, and systemic barriers for appropriate lead testing. Based on identified barriers we developed a key driver diagram (Fig 1) and implemented the following interventions using a Plan-Do-Study-Act model: a didactic on lead guidelines presented to all residents, reminders for testing posted in clinic, workflow for lead follow-up with easy-to-use tools integrated into the EMR. Lead testing rates were assessed monthly.
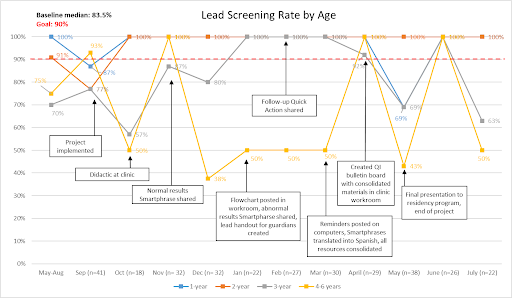
Results: Prior to our interventions, 83% of children 2 to 6 years old were appropriately tested for lead. During the QI project, the median testing rate for children 2-6 years old improved to 88%. One month after project completion, 73% of children 2-6 years old were appropriately tested, as seen in the annotated run chart (Figure 2). Universal testing of 2 year olds was sustained at 100% after project implementation. Universal testing of 3 year olds was more variable, with initial improvement that was not sustained. There was also variability in testing rates of high-risk 4-6 year olds due to the low number of patients in this category.
Conclusion(s): This QI project shows that it is possible to improve the rate of appropriate lead testing in a busy resident clinic by creating a workflow embedded in the EMR with tools to aid in implementation. Continued work needs to be done to sustain appropriate testing in 3-6 year olds at risk, and to evaluate appropriate follow up and management of lead testing results.