Adolescent Medicine
Session: Adolescent Medicine 1
146 - Telehealth versus in-person instruction for adolescents and young adults initiating gender-affirming testosterone therapy
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 146
Publication Number: 146.445
Publication Number: 146.445

Scott K. Jelinek, MD, MPH, MAEd (he/him/his)
Adolescent Medicine Fellow
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: The COVID-19 pandemic accelerated the adoption of telehealth services in the U.S. healthcare system, presenting new opportunities for the approximately 700,000 transgender adolescents and young adults (AYAs) aged 13-25 who often face significant healthcare barriers. This study evaluates the transition from in-person to telehealth testosterone injection instruction, a crucial aspect of transgender healthcare.
Objective: To compare the clinical effectiveness, time from prescription to injection, and incidence of post-instruction contacts for injection-related issues between telehealth and in-person instruction methods.
Design/Methods: Utilizing electronic health records from a large pediatric medical system, we conducted a retrospective cohort study of AYAs initiating testosterone (T) injections between March 1, 2018, and February 28, 2022. Patients were excluded if they were prescribed T.enanthate auto-inject or did not have documented injection teaching. Chi-square tests assessed demographic differences, while multivariable logistic and linear regressions, along with a zero-inflated negative binomial model, evaluated clinical effectiveness, time to treatment, and post-instruction contacts, respectively. The study was adequately powered to detect meaningful clinical differences.
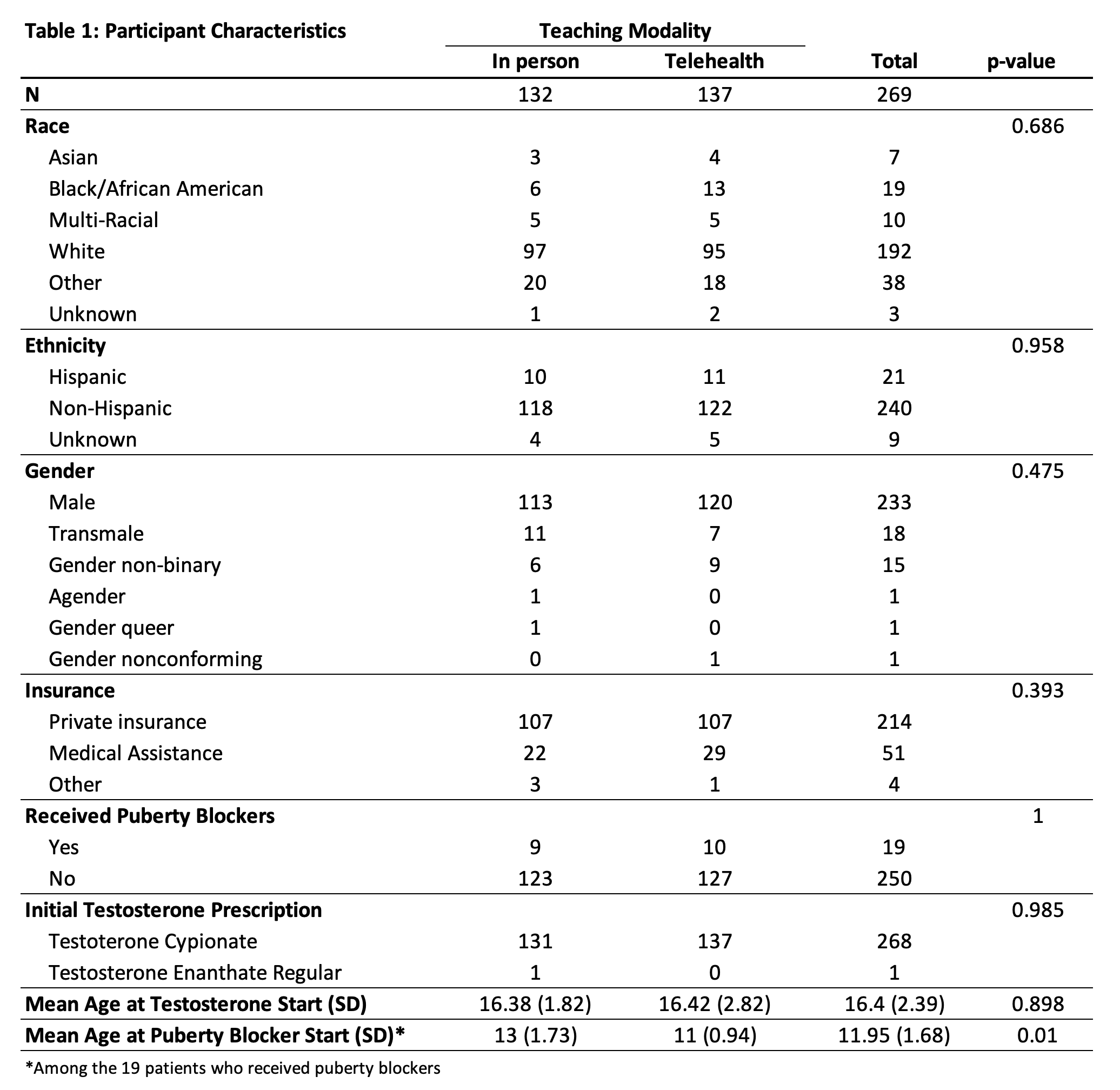
Results: Of the 269 participants (132 in-person, 137 telehealth), the mean age was 16.4 (± 2.39), most were non-Hispanic (89.2%), white (71.4%), commercially insured (79.6%), and had not used puberty blockers (92.9%), with no significant demographic differences between groups (Table 1). Clinical effectiveness, indicated by T levels at 3 and 6 months, revealed no significant difference between instruction methods (p=0.781 and p=0.213) after controlling for race/ethnicity, insurance type, use of puberty blockers, age, and whether the T prescription remained the same for the duration of the study. Time to treatment initiation was comparable (in-person: 15.02 ±15.03 days; telehealth: 17.82 ±15.87 days), with no significant difference in adjusted analysis (p=0.899). Post-instruction questions/problems were infrequent and similar between groups (in-person: mean of 0.18 ±0.47; telehealth: 0.14 ±0.40), with no significant differences in adjusted analysis (p=0.092).
Conclusion(s): Telehealth and in-person instruction for T injections are comparably effective for AYAs initiating gender-affirming care. Telehealth offers a viable alternative to in-person care, ensuring access to gender-affirming treatments, particularly for AYAs in remote areas or those preferring virtual healthcare due to potential discrimination in traditional settings.