Breastfeeding/Human Milk
Session: Breastfeeding/Human Milk 1: Breastfeeding
474 - Examining the Effects of Social Determinants of Health and Remote Outreach on Breast Milk Feeding Outcomes and Well Visit Completion Rates
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 474
Publication Number: 474.2063
Publication Number: 474.2063
- BF
Benjamin Foley, Bachelors of Science (he/him/his)
research coordinator
Cincinnati Children's Hospital Medical Center
Bellevue, Kentucky, United States
Presenting Author(s)
Background: Breast milk is the normative standard for infant nutrition and is linked to positive health benefits for both the infant and mother. During the start of the COVID-19 pandemic, there were less in-person well and follow-up visits. The fewer visits raised concern about insufficient support for newborns, especially those receiving breast milk in a pediatric clinic where 72% of patients were African American and 72% had Medicaid insurance. Thus, a remote breastfeeding support program was created and caregivers completed a health related social need screen (HRSN) to help identify barriers that may negatively impact their infant.
Objective: To examine the effect of HRSNs on breastmilk feeding rates, engagement in BF support, and well visit completion rates at the 2, 4, and 6 month well visit.
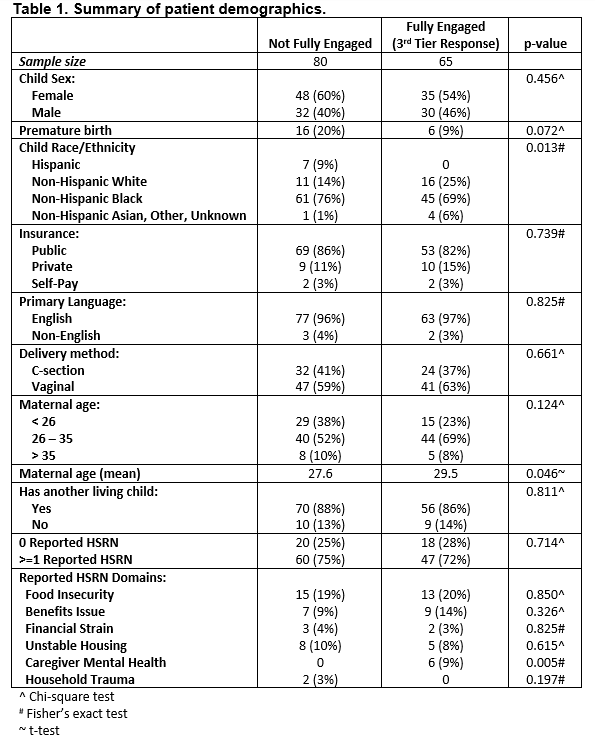
Design/Methods: Breast milk feeding (BMF) support intervention was provided to mothers of infants seen for newborn well visits (NWVs) from 9/28/20 – 2/19/21. Infants seen for NWVs with a completed HRSN screen and receiving any breastmilk were contacted for remote breastfeeding outreach. Follow-up data was collected on BMF status and well-visit completion rates at 2, 4, and 6 months of age and data was analyzed using logistic regression.
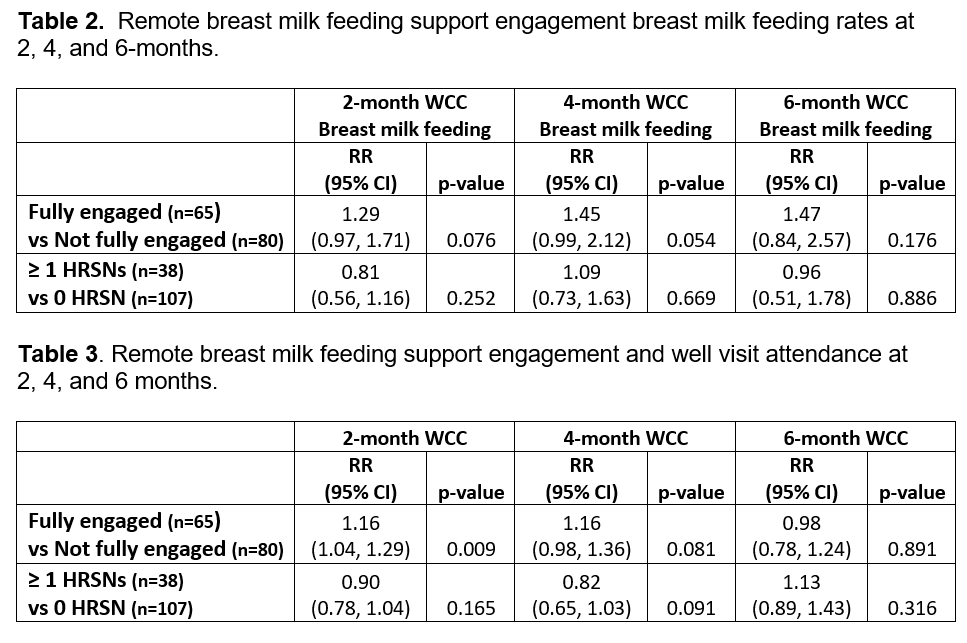
Results: In this study population comprising 246 infants, 59% were receiving breastmilk at their newborn visit and 25% were in households with at least 1 HRSN . Community health workers attempted to contact 100% of mothers who provided BMF to their newborns, 88% of mothers confirmed their phone number, 60% confirmed the feeding status, and 45% participated in remote BMF support. While remote BMF support did not significantly increase breast milk feeding rates, it did significantly increase return for the 2 month well child visit (RR=1.16, 95% CI 1.04, 1.29), after adjusting for the presence of at least one social risk.
Conclusion(s): This study demonstrates a novel approach integrating community health worker text-based outreach and remote lactation support within a primary care clinic to assist breastfeeding mothers. We show that mothers who were fully engaged in a remote lactation support outreach program were significantly more likely to return to primary care clinics with their infants for a 2-month well child check as compared to mothers who were not fully engaged in the program. They were also 45% more likely to still be breastfeeding their infants at 4 months (p=0.054).