Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 1
361 - Increasing the proper placement of gastric tube in the neonatal intensive care unit: a quality improvement program
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 361
Publication Number: 361.2018
Publication Number: 361.2018
Huayan Zhang, MD
Neonatologist
Children's Hospital of Philadelphia/Guangzhou Women and Children's Medical Center
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Although frequently used, previous studies showed 44%-59% of neonatal nasogastric or orogastric (NG/OG) tubes were located in improper position which may lead to serious complications including iatrogenic gastric perforations, aspiration pneumonia and other pulmonary diseases.
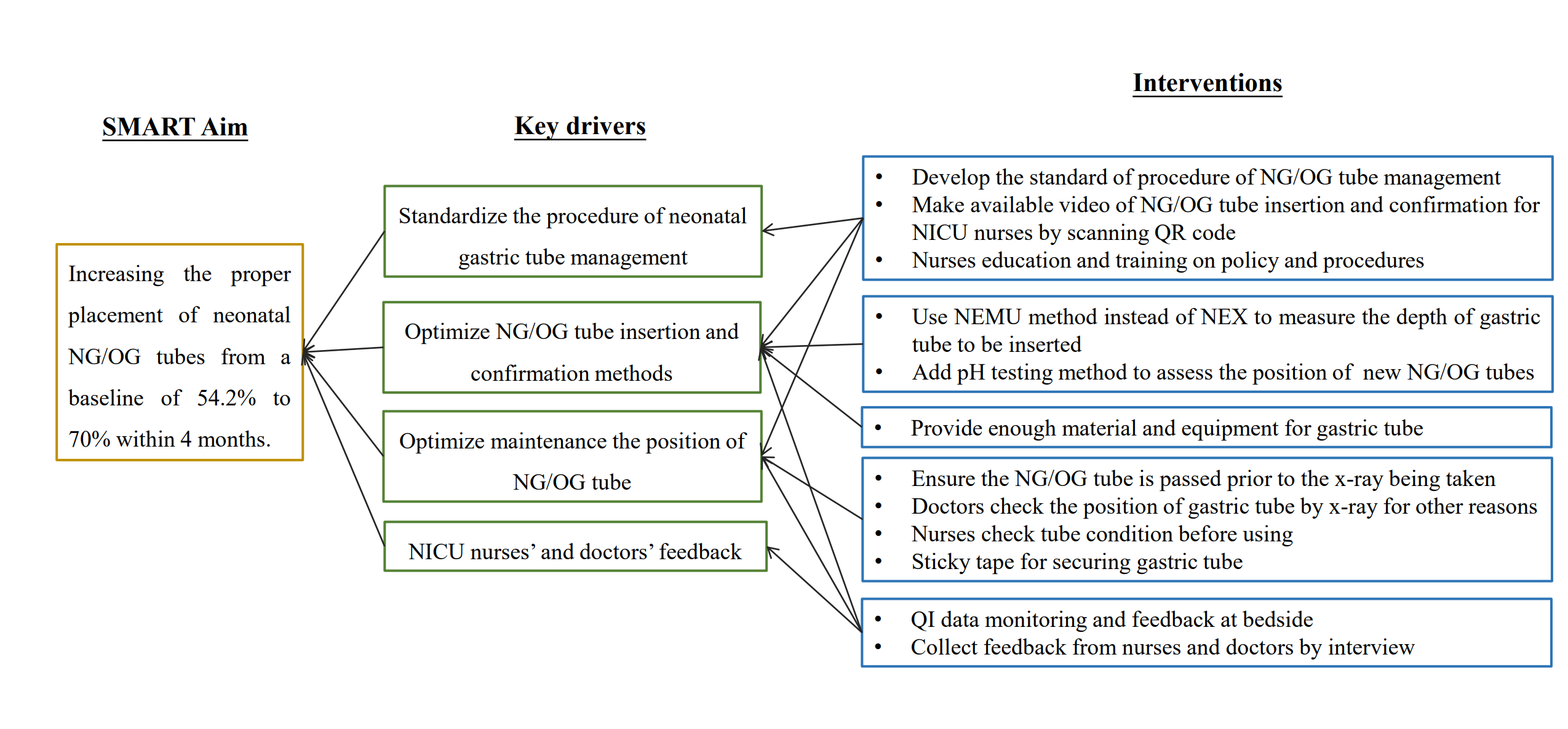
Objective: Increasing the proper placement of neonatal NG/OG tubes from a baseline of 54.2% to 70% within 4 months.
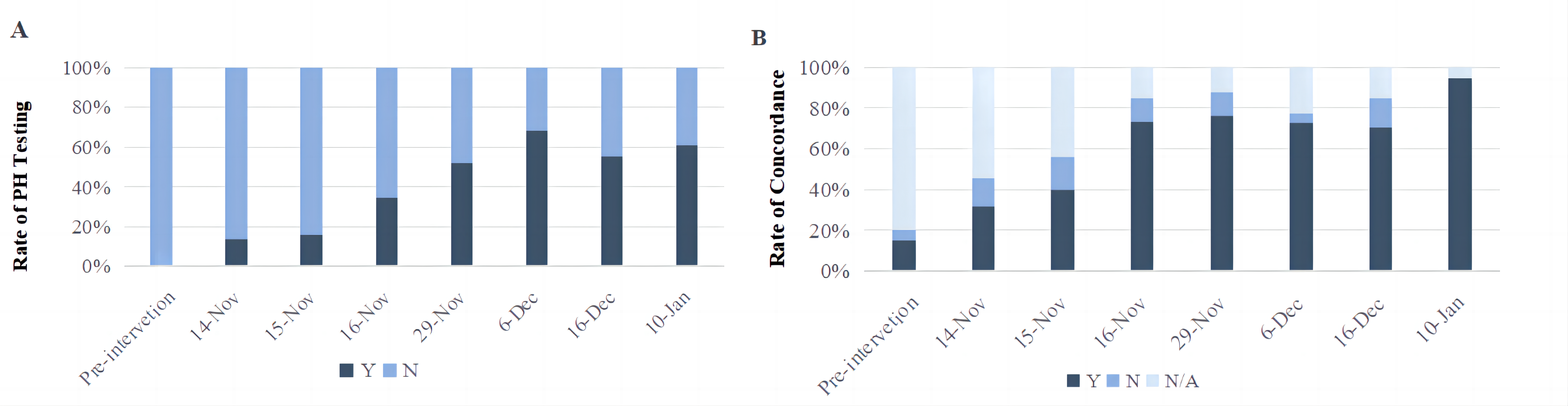
Design/Methods: This quality improvement project was conducted from October 2022 to January 2023 in a 90-bed level IV NICU at Guangzhou Women and Children’s hospital. A Key Driver diagram (Figure 1) was used to guide interventions and PDSA (Plan, Do, Study, Act) cycles. PDSA Cycles mainly involved 1) revised the standard of procedure (SOP) of neonatal NG/OG tube management based on clinical guidelines and current best evidences; 2) educated and trained nurses on the optimal method to measure the length of NG/OG tube and confirm NG/OG tube placement by small-group workshops; 3) Optimized maintenance of the NG/OG tube position; 4) collected NICU nurses’ feedback by focus group interview. The primary outcome measure was the percentage of proper NG/OG tube placement as assessed by x-ray. Data were collected every 2 days. Control charts were used to track time ordered data and detect special cause variation. Process measures included 1) rate of gastric pH testing documented at the time of NG/OG tube insertion 2) the concordance rate between the actual and labeled depth of gastric tube in neonates per day. Gastric bleeding and gastric perforation associated with gastric tube placement and increased workload of NICU nurses were followed as balancing measures.
Results: During the QI period, 284 neonates with NG/OG tube placement were observed. the proper placement per 2 days increased from 54.2% to 77.29% (Figure 2). Rate of gastric pH testing at the time of insertion increased from 0% to 61.11%. The concordance rate between the actual and labeled depth of gastric tube in neonates increased from 31.82% to 94.44%. Complications were minimal and increased workload were acceptable to the nurses.
Conclusion(s): The proper placement of neonatal gastric tube was increased by focusing on standardized the gastric tube management including optimize NG/OG tube insertion and confirmation methods, nurses’ education and training, as well as nurses and doctors’ attitude and feedback.
.png)