Emergency Medicine
Session: Emergency Medicine 6: Airway and POCUS
207 - Using Point of Care Ultrasound (POCUS) to Assess Gastrostomy Balloon Placement
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 207
Publication Number: 207.2041
Publication Number: 207.2041
.jpg)
Nithin Ravi, MD
Pediatric Emergency Fellow
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background: Fluoroscopy is the gold-standard for evaluation of gastrostomy tube (GT) placement. Fluoroscopy is resource intensive and exposes patients to contrast and radiation. Ultrasound has yet to be rigorously evaluated as a low-risk alternative to confirm GT placement.
Objective: To determine the diagnostic accuracy of point of care ultrasound (POCUS) for identification of correct gastrostomy balloon placement as compared to fluoroscopy.
Design/Methods: This was a prospective diagnostic accuracy study. Recruitment included a convenience sample of children presenting to interventional radiology for routine gastrostomy (GT) or gastrojejunal (GJ) tube exchange. Prior to exchange, a POCUS scan was performed by a novice pediatric or pediatric emergency medicine physician, followed by a fluoroscopic study. Ultrasound images were interpreted by the POCUS operator and a POCUS expert independently. A certified radiologist interpreted all fluoroscopic studies. The POCUS exert and radiologist were masked to the POCUS operator interpretations prior to their independent assessments of GT/GJ balloon placement. Diagnostic test characteristics with 95% confidence intervals and interrater agreement (Cohen’s Kappa) between POCUS and fluoroscopy were calculated. Factors influencing POCUS interpretation were assessed using logistic regression.
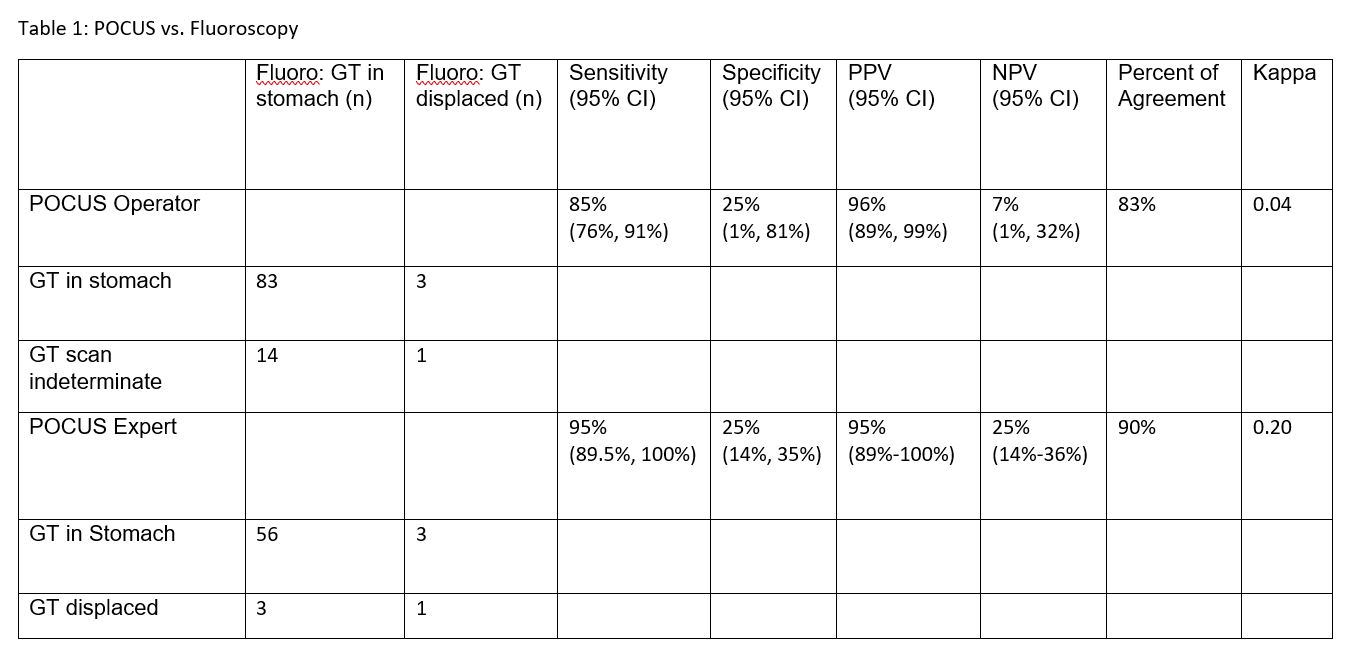
Results: Of 101 patients enrolled, 4 (4%) gastrostomy balloons were displaced. Novice POCUS interpretations of GT/GJ balloon placement, when compared to fluoroscopy, demonstrated a sensitivity of 85% (76%, 91%), specificity of 25% (1%, 81%), PPV of 96% (89%, 99%), NPV of 7% (1%, 32%), proportion agreement of 83%, kappa 0.04. Official POCUS expert interpretation, compared to fluoroscopy, showed higher sensitivity of 95% (89.5%, 100%), proportion agreement of 90%, kappa 0.20. Higher BMI [0.76 (0.62, 0.92)] and older age [0.88 (0.80, 0.94) decreased the odds of determining placement by the novice POCUS provider.
Conclusion(s): POCUS had a high sensitivity for GT/GJ balloon placement, but low concordance and interrater agreement, suggesting POCUS may not add clinical utility compared to gold-standard fluoroscopy. POCUS expertise increased diagnostic accuracy for GT/GJ placement. Interpretation of PPV, NPV, and specificity were limited by a low number of displaced gastrostomy balloons.