Mental Health
Session: Mental Health 1
558 - Impact of COVID-19 on Acute Care Hospitalizations for Suicidality: How did Patients Differ by Race, Socioeconomic Status, and Re-utilization?
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 558
Publication Number: 558.1982
Publication Number: 558.1982

Sarah H. Vepraskas, MD (she/her/hers)
Associate Professor
Medical College of Wisconsin
Medical College of Wisconsin
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: Prior to the COVID-19 pandemic, pediatric hospitals reported a concerning trend in hospitalizations related to psychiatric illness. The pandemic amplified the rates of mental health disorders in young and farther contributed to a public health crisis for child and adolescent mental health. Noting an increase in patients presenting with suicide ideation (SI) and suicide attempts (SA), we sought to farther characterize this population.
Objective: Our objectives were: 1. Compare the frequencies of hospitalizations for suicidality before and after the onset of the COVID-19 pandemic to determine whether they differed by age, sex, race/ethnicity, or SES; 2. Assess admission trends during the COVID-19 surges; 3. Examine and compare 7, 30, and 365-day re-utilizations rates.
Design/Methods: Retrospective data between January 2017 and March 2022 was analyzed, including patients ages 10-17 hospitalized for suicidality on the critical care and acute care services. Encounters were divided into 2 categories based on the COVID-19 pandemic: “pre-lockdown” (1/17-2/20) and “post-lockdown” (3/20-3/22). We analyzed numerical frequencies using means and standard deviations, categorical data using chi-square tests and Fisher’s exact tests, and continuous data with t-tests and Mann-Whitney U tests. P values of < 0.05 were considered significant.
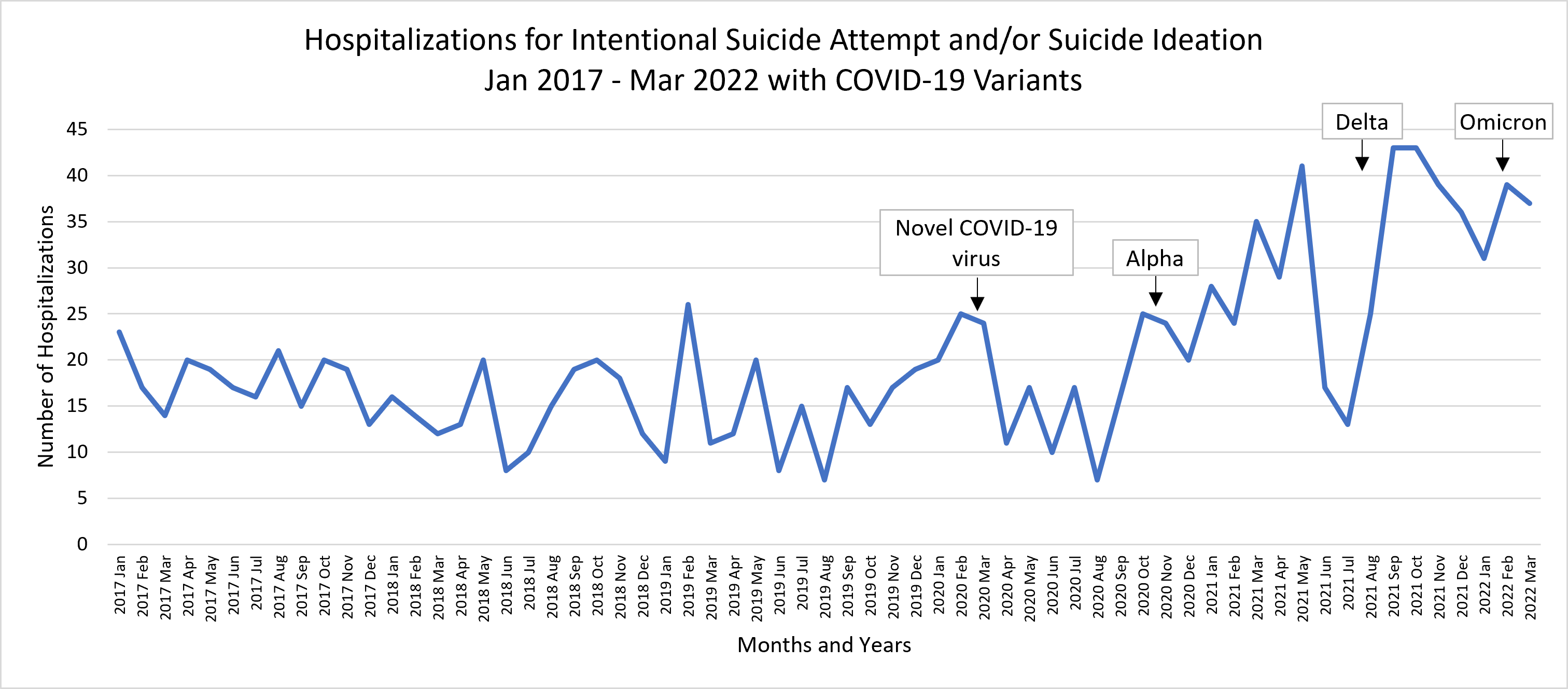
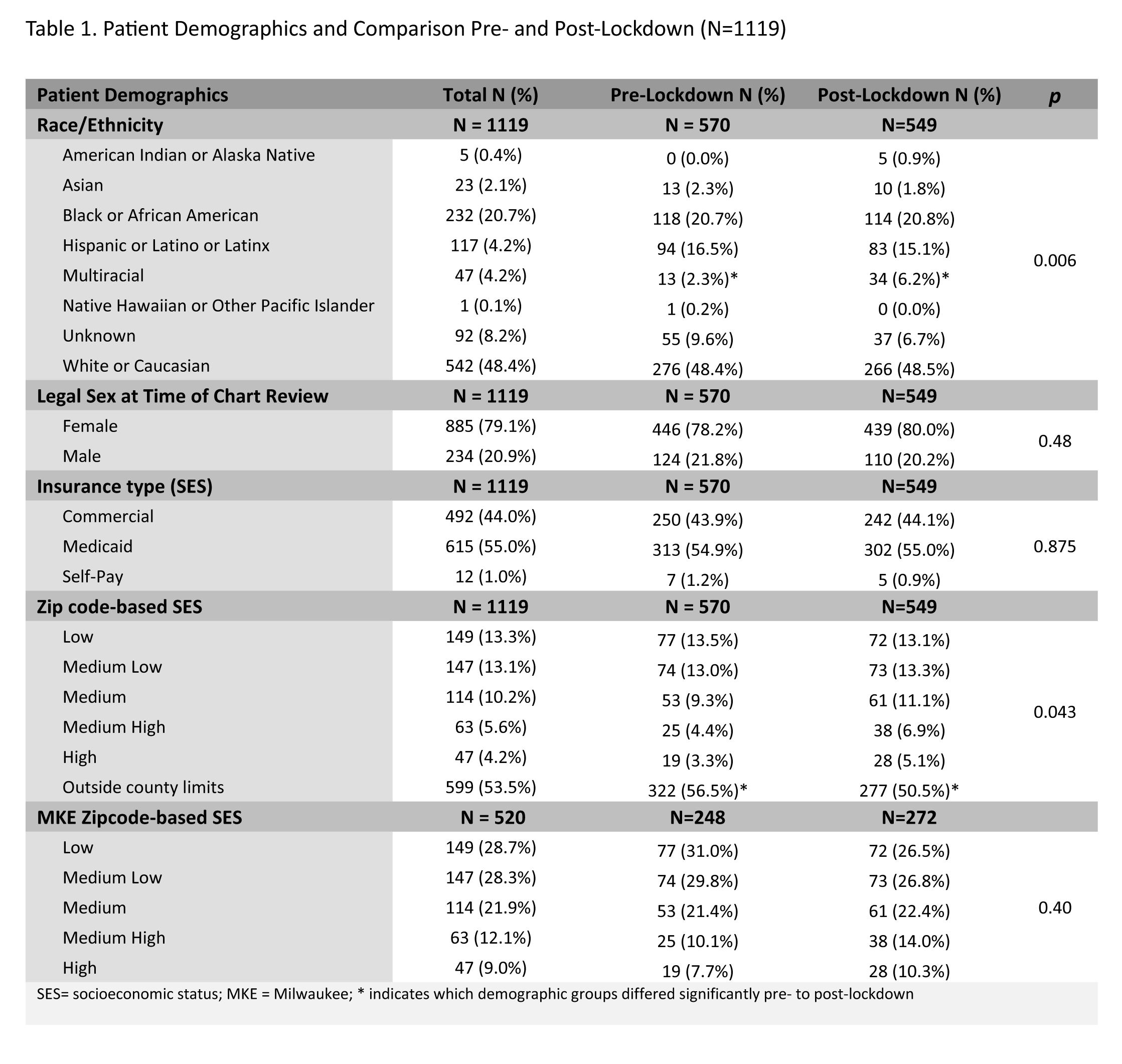
Results: 1261 encounters were included. Once stratified into our pre and post lockdown groups for analysis, there were 1139 encounters and 1119 unique patients. There was a statistically significance difference in multiracial patients post-lock-down (P=0.006), as well as fewer patients from outside the hospital’s county (P=0.043) (Table 1). There was no significant difference in 7- and 30-day ED visits or readmissions pre- versus post lockdown (Table 2). There were significant differences in those who presented to the ED and readmitted over 365 days pre- and post-lockdown, making the 365-day re-utilization statistically significant (P=0.027) (Table 2). A chronological visual representation of total encounters with the COVID-19 surges annotated (Novel Coronavirus-19 (3/20), Alpha (9/20), Delta (8/2021) and Omicron (1/22)) was generated (Figure 1).
Conclusion(s): Our study suggests the COVID-19 pandemic has further intensified the already critical issue of mental health in our youth, demonstrating an escalation in admissions following COVID surges, increased re-utilization in the year following their initial presentation, and a significant increase in multiracial youth presenting after the pandemic. Our findings can help us formulate plans for future targeted interventions.
.jpg)
