Neonatology
Session: Neonatal/Infant Resuscitation 1
265 - Navigating ETT Depth: Surfactant Administration in the Delivery Room for Very Preterm Infants
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 265
Publication Number: 265.3059
Publication Number: 265.3059

Kelsey Wigand, B.S
Medical Student
Medical College of Wisconsin
Muskego, Wisconsin, United States
Presenting Author(s)
Background: Surfactant therapy is crucial for very preterm infants requiring mechanical ventilation for severe respiratory distress syndrome (RDS), with its success hinging on precise endotracheal tube (ETT) placement. Various methods exist for determining ETT depth, including gestational age-dependent measurements and nasal tragus length, but radiographic confirmation remains the gold standard. We hypothesize that these preterm infants receive more surfactant in the neonatal intensive care unit (NICU) than in the delivery room (DR).
Objective: To compare the demographics, labor and delivery (L&D) characteristics, and outcomes of infants who got the first dose of surfactant in the DR versus the NICU. To determine the different methods and challenges of correct ETT depth in the DR.
Design/Methods: A retrospective chart review of ≤32 weeks gestation (GA) and intubated in DR infants admitted to a level 4 NICU from 01/2021- 12/2022. In 06/2023, we surveyed neonatal providers (NP) using a non-probability convenience sampling method. The survey consisted of questions to assess preference for ETT depth measurement and position, and challenges of administrating surfactant in the DR. For analysis, we compared the demographics, L&D characteristics, and outcomes of DR vs. NICU surfactant using the Chi-square and Fisher's exact tests, Mann-Whitney, or Students T-tests.
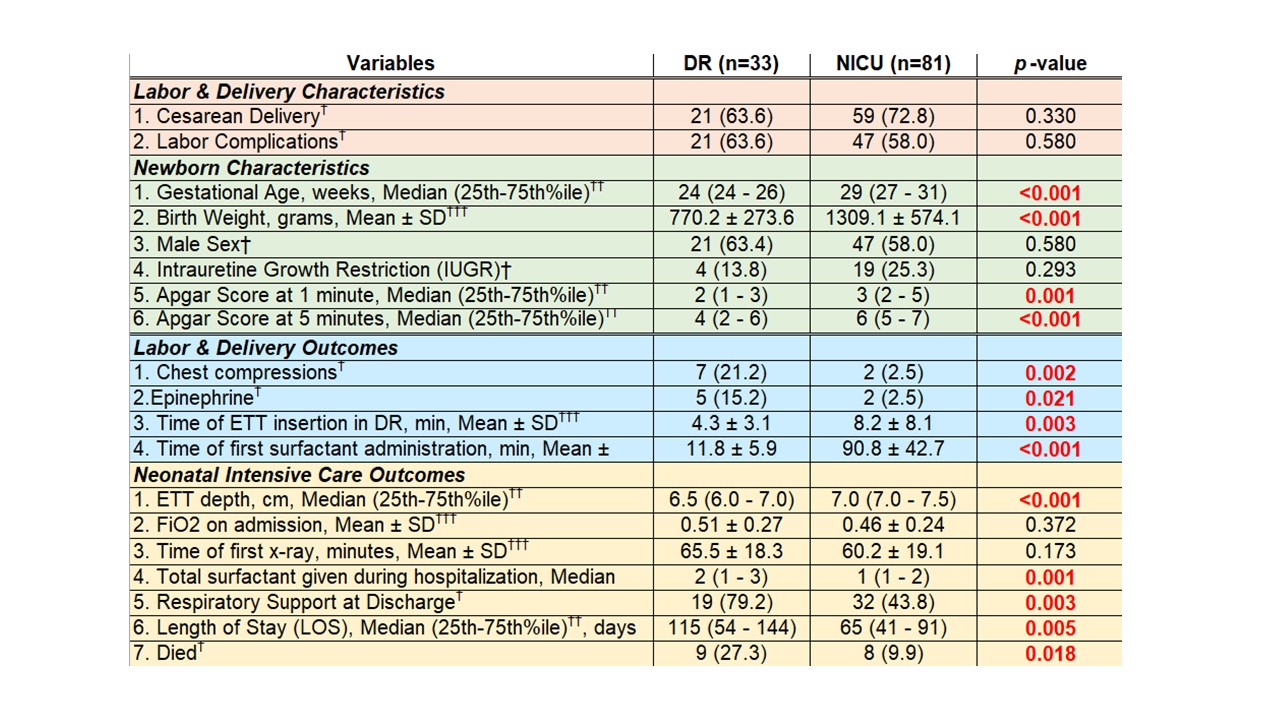
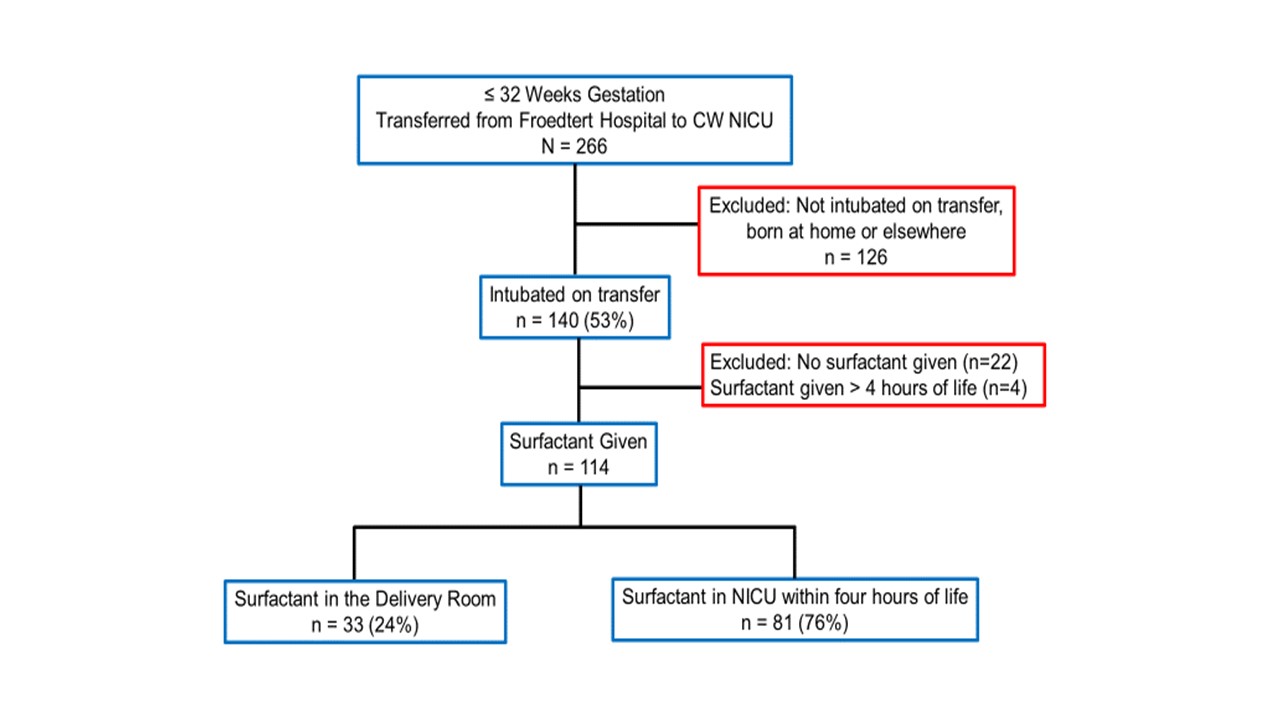
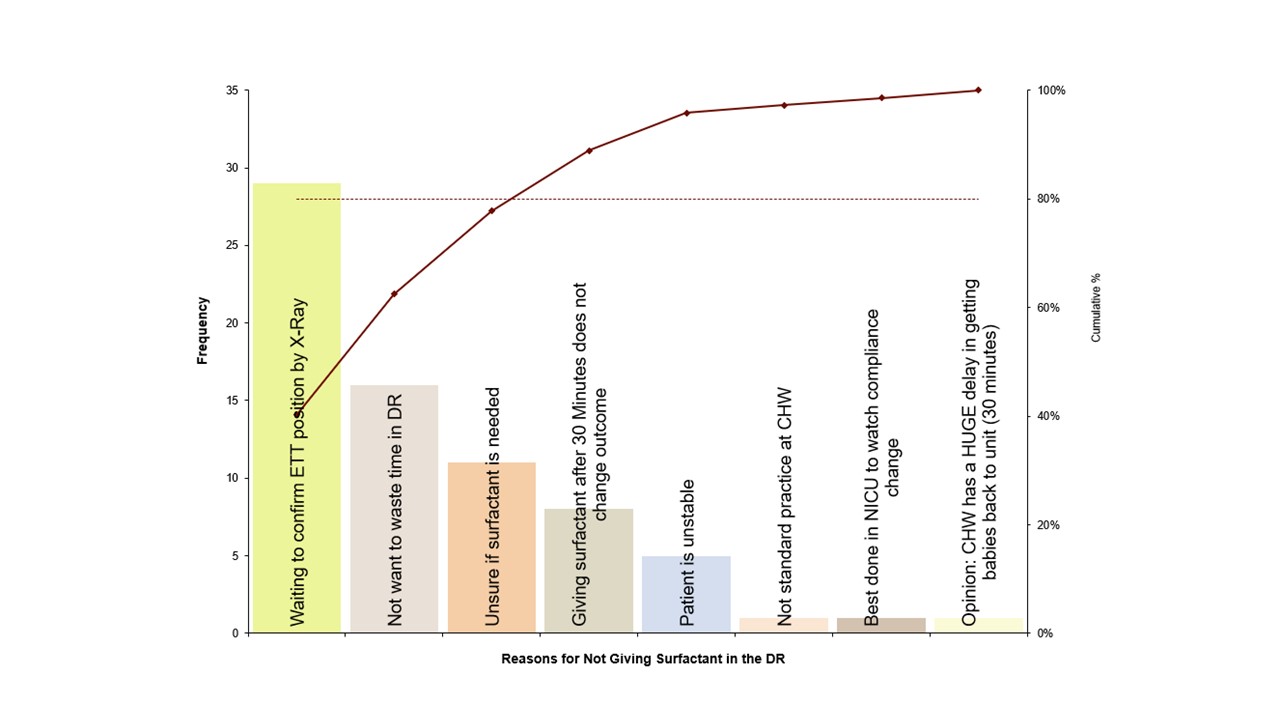
Results: Out of 266 infants, 53% were intubated in DR (Fig: 1). Of those, 84% received surfactant, but only 29% in the DR. Infants in the DR surfactant group were younger, had lower birth weight, and had lower Apgar scores (Table 1). There was similar ETT depth location for both groups [between thoracic inlet and above carina (51%), below carina (12%), at carina (22%), and above thoracic inlet (15%)]. The two groups' mean FiO2 on admission was similar. Infants who got DR surfactant had more surfactant doses given, higher deaths, longer length of stay (LOS), and required more respiratory support at discharge. Out of 42 survey respondents, 49% use Tochen’s formula, and 40% would only give surfactant after x-ray confirmation (Fig: 3).
Conclusion(s): Our findings underscore challenges surrounding DR surfactant administration where infants were younger, smaller, and more unstable at birth. We speculate that DR surfactant is given as a rescue medication. Among NPs, Tochen’s formula is the predominant choice of ETT depth measurement, and surfactant administration in the NICU after radiographic confirmation is preferred. Our next step includes formulating and implementing a consistent method for ETT depth measurements and surfactant administration guidelines.