Neonatology
Session: Neonatal General 4: Nutrition, Feeding, and Growth
102 - Impact of using preterm formula higher in protein and whey content on feeding intolerance in very low birthweight infants
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 102
Publication Number: 102.298
Publication Number: 102.298

Cole Turner, DO (he/him/his)
Neonatal-perinatal Medicine Fellow
New York University Grossman School of Medicine
New York, New York, United States
Presenting Author(s)
Background: Formula is the primary source of protein for very low birthweight (VLBW) infants when human milk is unavailable; formulas have varying levels of protein and ratios of milk proteins, whey and casein. Whey has been demonstrated to be more rapidly digested and is associated with faster gastric emptying and softer stools, whereas casein aggregate into curds thus delaying delivery of constituent metabolites to the intestine. We hypothesize that a formula with higher protein/whey content will improve feeding tolerance, improve growth and decrease the need for modulars, liquid protein (LP) and medium chain triglyceride oil (MCT) in VLBW infants.
Objective: The primary objective was to determine the impact of higher protein/whey formula on feeding tolerance in a cohort of VLBW preterm infants from initiation of formula until NICU discharge, with secondary objectives of observing the impact on growth and modular usage in the same cohort.
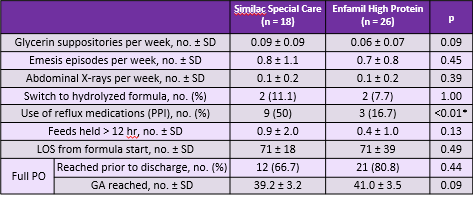
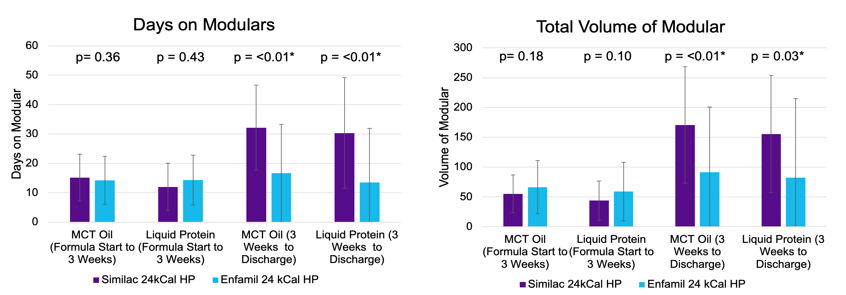
Design/Methods: This was a retrospective chart review of VLBW infants defined as < 28 weeks gestational age and < 1500g. The infants were divided into 2 groups: 1) infants who fed a 24kcal preterm formula with 3.3g protein and a 60/40 whey/casein ratio versus 2) infants who fed a 24kcal preterm formula with 3.6g protein and a 80/20 whey/casein ratio. Feeding intolerance was defined as the need for glycerin suppositories, feeds being held >12 hours, use of a reflux medication, changing to a hydrolyzed formula, emesis episodes and abdominal radiographs ordered. We also compared length of stay, time to reach full enteral feeds, use of LP and MCT modulars and growth metric z-scores between the two groups.
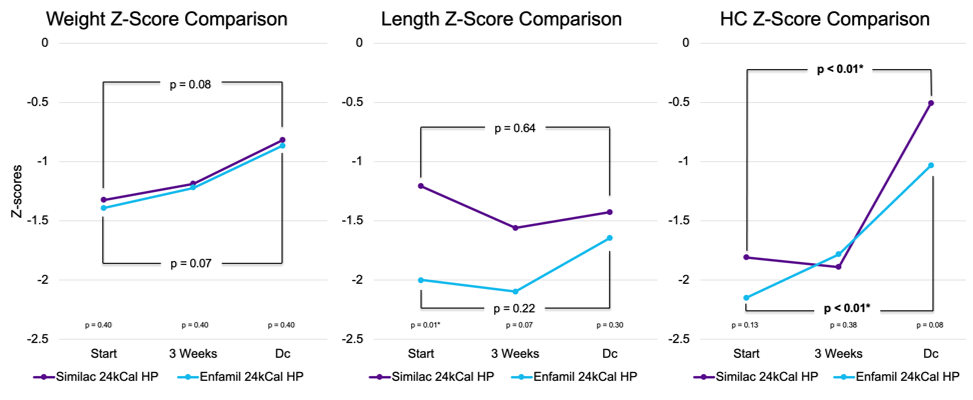
Results: There were no significant differences in our markers for feeding intolerance between the two groups with the exception of the group with higher protein/whey content formula receiving less reflux medication (Figure 1). Additionally, while no significant changes in growth between the two groups were observed, those infants receiving the higher protein and whey formula showed improved trends in length and head circumference (Figure 2) and had a significantly decreased usage of modulars (Figure 3).
Conclusion(s): As most VLBW infants are discharged on a feeding plan that involves formula, our study supports that a formula higher in protein and whey content could be beneficial. Our study supports that higher protein and whey content formulas are tolerated as well, if not better than lower protein whey content formulas. Additionally, they could support better growth, as demonstrated from our observed trends in length and head circumference as well as the decreased need for modulars.