Neonatology
Session: Neonatal Pulmonology - Clinical Science 6: Respiratory/Neuro Outcomes, Steroids
591 - Bayley Scores at 24 Months in Severe Bronchopulmonary Dysplasia Patients with and without a Tracheostomy
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 591
Publication Number: 591.2751
Publication Number: 591.2751
.jpg)
Audrey Miller, MD
Assistant Professor
Ohio State University College of Medicine and Nationwide Children’s Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background: Infants with severe bronchopulmonary dysplasia (BPD) may require chronic invasive ventilation necessitating tracheostomy. Specific criteria for and timing of tracheostomy remain uncertain. Neurodevelopmental outcomes are often an influencing factor in the decision to proceed with tracheostomy, even in the setting of limited evidence that describes the association of tracheostomy with neurodevelopmental impairment in BPD.
Objective: To determine if infants with BPD and a tracheostomy had significantly differing neurodevelopmental outcomes at 24 months corrected age compared to infants with BPD and no tracheostomy.
Design/Methods: A single center observational study including all patients diagnosed with severe BPD admitted to our BPD unit from 2010 to 2020. Severe BPD was defined as oxygen treatment for at least 28 days with an oxygen requirement above 30% and/or the need for positive pressure ventilation at 36 weeks post-menstrual age. There were 288 patients identified with severe BPD that had any Bayley score available at 24-month follow-up, of which 15 (5.2%) had a tracheostomy and 273 (94.8%) did not have a tracheostomy.
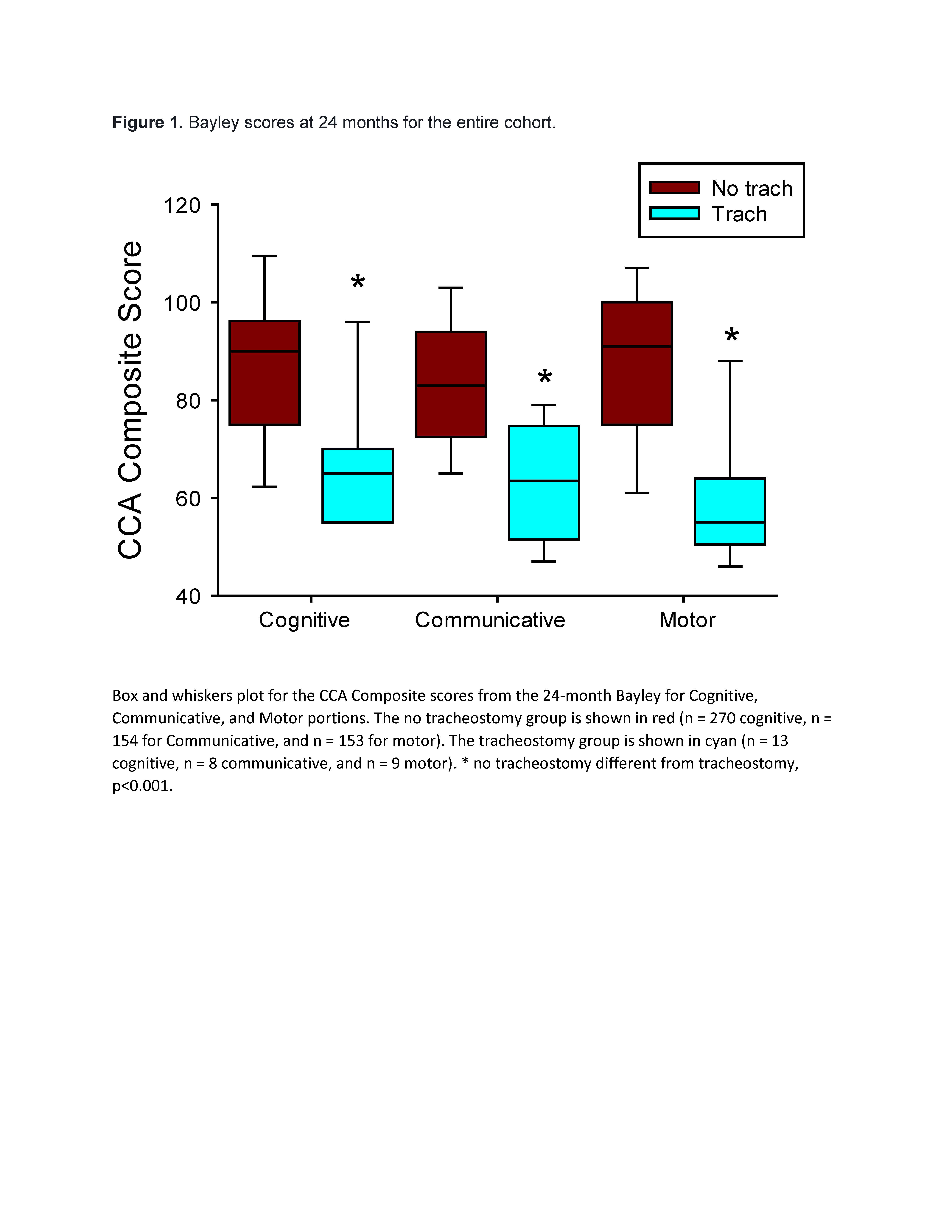
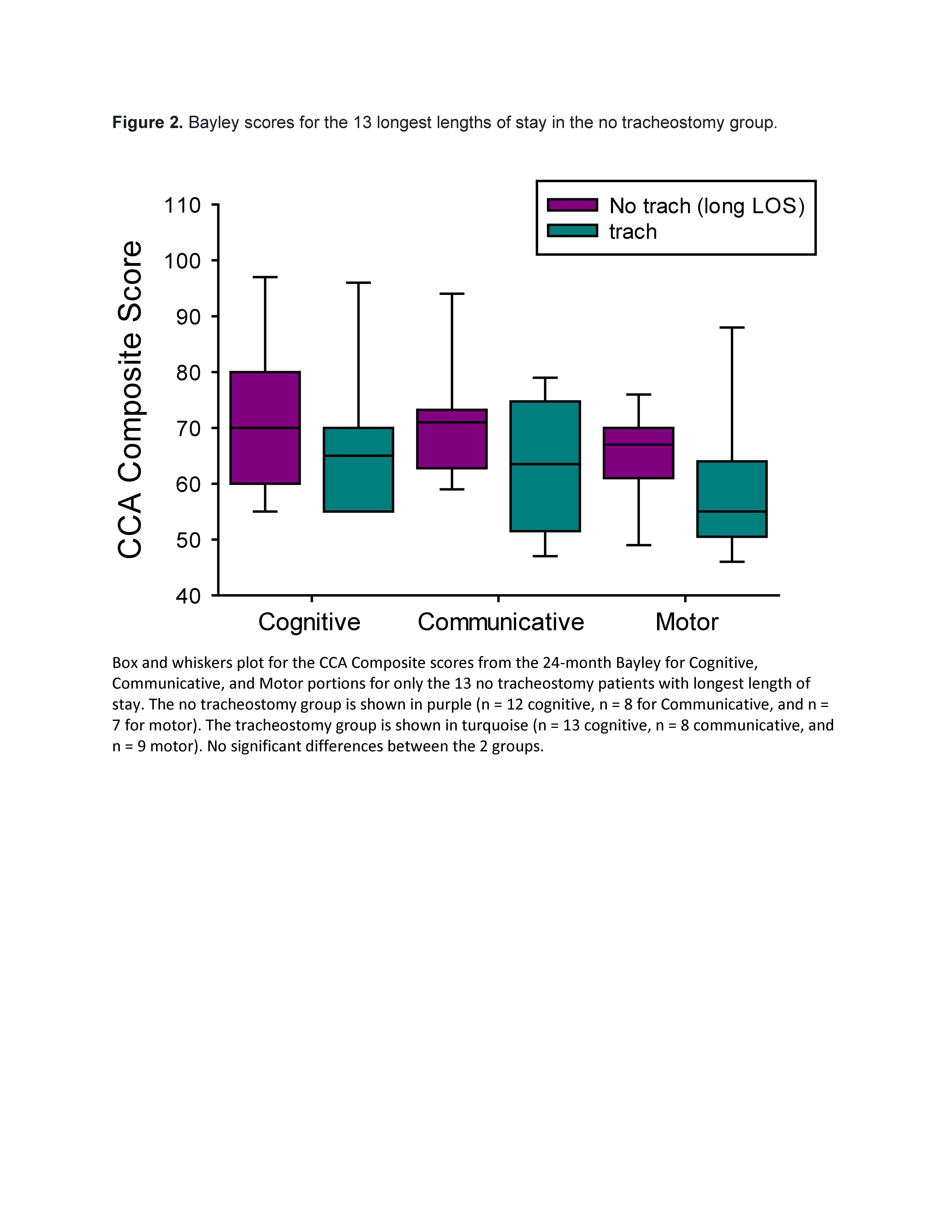
Results: The 24-month Bayley scores for the patients with a tracheostomy were significantly (p < 0.001) lower than in patients without a tracheostomy (Figure 1). The gestational age at birth and the birth weight did not differ between the two groups. The median length of stay was significantly longer (p < 0.001) in the patients with a tracheostomy (418 (IQR 303 – 675)) than in those without a tracheostomy (140 days (IQR 106 – 189)). When only the 13 no tracheostomy patients with the longest lengths of stay (median 323 days (IQR 314 – 403)) were included, there were no differences in 24-month Bayley scores between the 2 groups (Figure 2).
Conclusion(s): Infants with BPD requiring tracheostomy had significantly lower Bayley scores compared to infants with BPD without tracheostomy. Furthermore, in this single center study with a low rate of tracheostomy, the subset of longest stay no tracheostomy patients did not have worse Bayley scores than patients with tracheostomy, suggesting tracheostomy avoidance may not be associated with worse neurodevelopmental outcomes even with long length of stay. This information may be helpful to help guide conversations surrounding tracheostomy decision making. Furthermore, these results underscore the need for evidence generating trials to understand if tracheostomy impacts neurodevelopment in severe BPD.