Asthma
Session: Asthma 2
205 - Exploring a best practice for reporting asthma-related mobile health data: A qualitative examination of clinical provider perspectives
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 205
Publication Number: 205.45
Publication Number: 205.45

Megan McDonald, BS (she/her/hers)
Medical Student
Medical University of South Carolina College of Medicine
Anderson, South Carolina, United States
Presenting Author(s)
Background: The emergence of mobile health (mHealth) has swept through the literature in virtually all fields resulting in an abundance of data for providers to review. Although guidelines exist regarding the development of mHealth applications, no studies have explored provider preference in asthma mHealth data reporting.
Objective: This study aimed to explore provider preference regarding best practice for reporting mHealth data related to asthma. We sought to produce a guideline for how mHealth asthma applications can best aid providers in caring for patients rather than inundating them with large amounts of data to interpret on their own.
Design/Methods: We utilized a qualitative, descriptive approach to perform standardized interviews with clinicians currently engaged in care for children with asthma. A standardized script was piloted for clarity and used in key informant interviews (KIIs). The goal of the KIIs was to isolate common themes regarding perceptions on the desired reporting of mHealth data for use in the clinical setting. Themes were isolated and coded based on interview transcripts by two independent investigators and any differences reconciled. Interviews were continued until thematic saturation was achieved. The project was approved by our Institutional Review Board for exempt-level review.
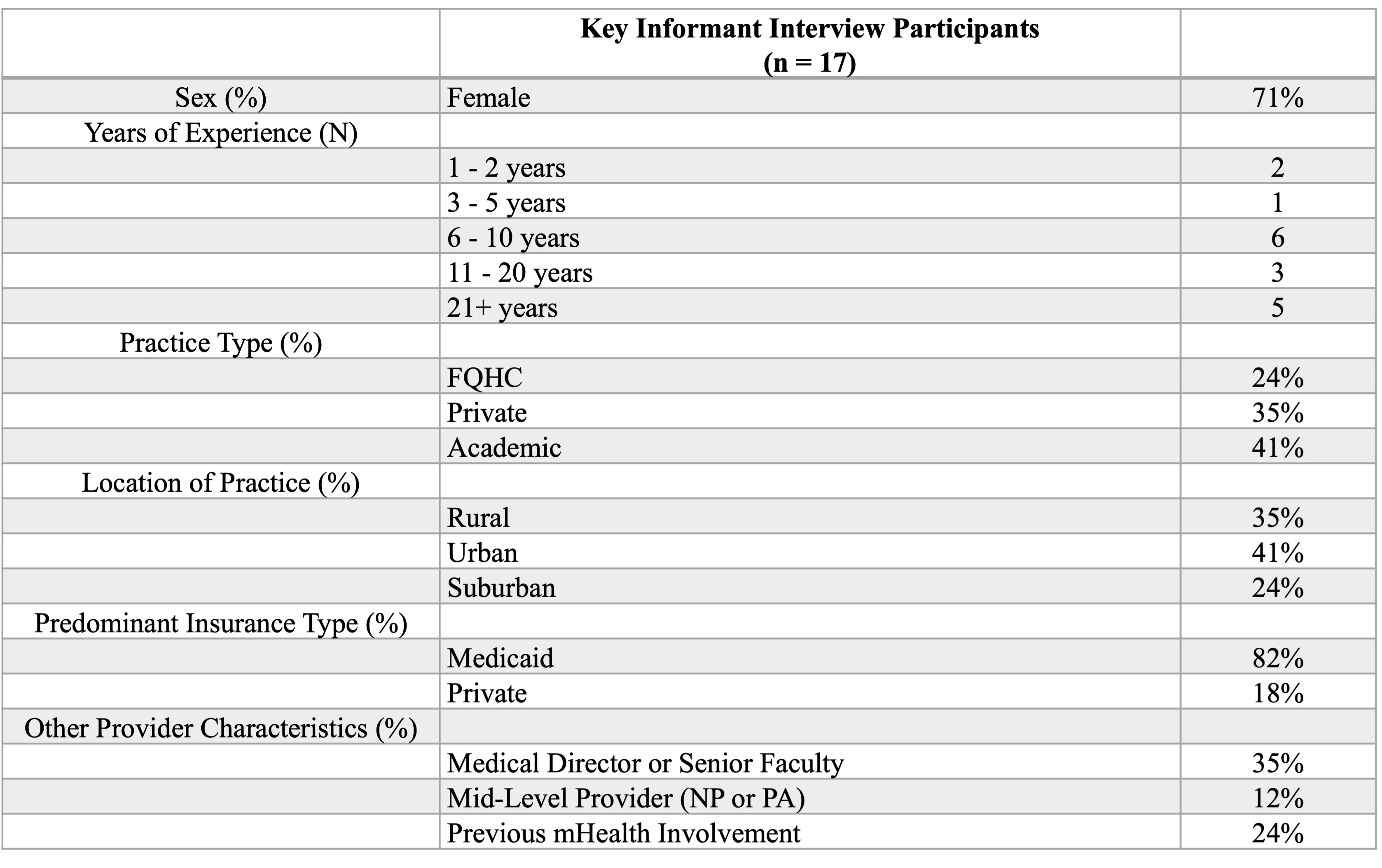
Results: A total of seventeen providers were interviewed. Participants consisted of twelve females and five males. Participants served primarily patients with Medicaid insurance and an adequate balance was achieved in practice location (rural vs. urban vs. suburban) and type (FQHC vs. academic vs. private).
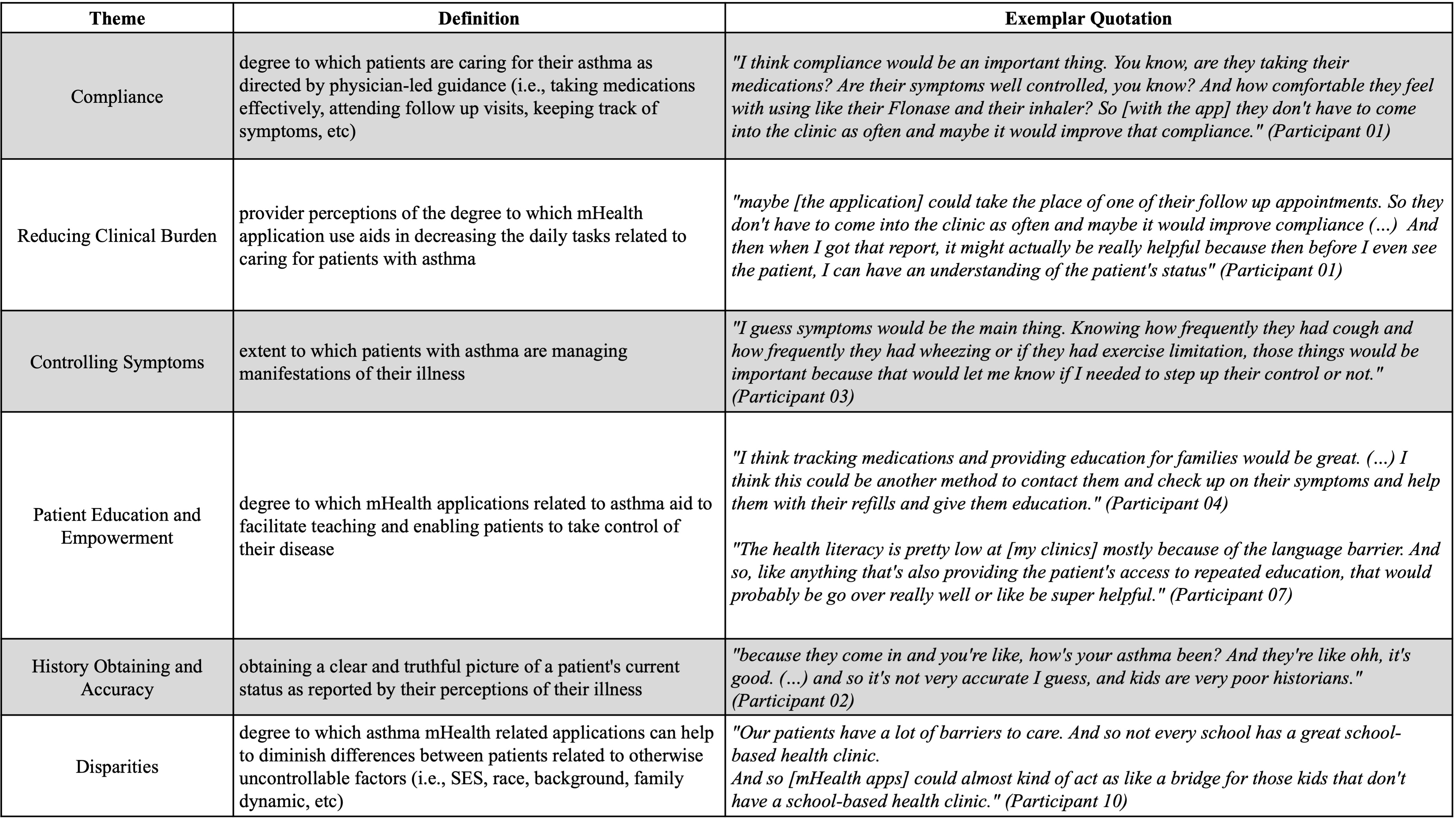
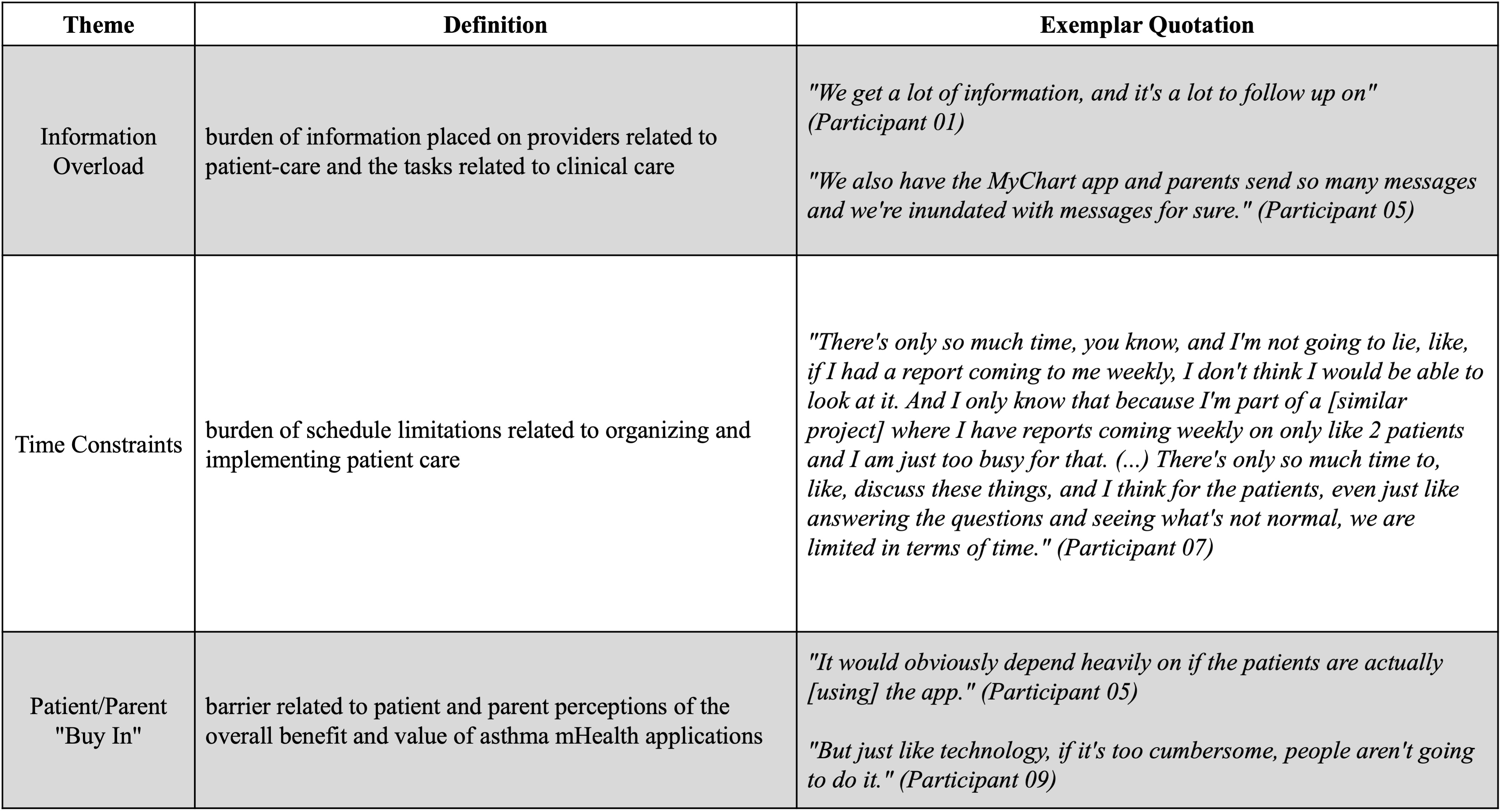
Major themes identified included compliance, reducing clinical burden, and patient education and empowerment as benefits of using mHealth applications; information overload, time constraints, and patient/parent buy-in as potential barriers. A desire for integration with the electronic medical record, objective measurements, and inclusion of red-flag criteria were crucial themes related to reporting.
Conclusion(s): Our study included overall support for mHealth applications related to caring for children with asthma and demonstrated clinicians’ desires as a means to improve the feasibility and practicality of implementation of mHealth into everyday practice. As mHealth app use expands and risks inundating providers with large amounts of data to interpret, these results inform guidelines to improve provider efficiency and care for children with asthma, helping to bridge the gap in asthma care, particularly in areas where there is a lack of providers or time available for distinct and detailed patient care.