Neonatology
Session: Neonatal Neurology 6: Clinical
561 - Epidemiology and clinical features of lissencephaly and holoprosencephaly among a large cohort of Texas infants
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 561
Publication Number: 561.1610
Publication Number: 561.1610
- SA
Samiya F. Ahmad, MD (she/her/hers)
Associate Professor of Pediatrics
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Due to their rarity, the descriptive epidemiology and clinical outcomes of many central nervous system (CNS) birth defects are poorly described. No large population-based studies have investigated sociodemographic and clinical characteristics associated with occurrence of major CNS defects in the United States.
Objective: We sought to identify the epidemiological factors associated with the occurrence of holoprosencephaly (HPC) and lissencephaly (LS) and to describe major clinical features of infants with these diagnoses as ascertained by a population-based active surveillance system.
Design/Methods: The Texas Birth Defects Registry (TBDR) conducts active surveillance of birth defects among pregnancy outcomes, i.e., cases, of mothers who are Texas residents at the time of delivery. We utilized the TBDR to identify cases HPC and LS between 1999 and 2015. Maternal demographics, infant characteristics, and clinical outcomes information of birth defect cases are extracted from a combination of birth certificates and medical records. Prevalence rates were expressed as cases per 10,000 live births. Prevalence ratios (PR) and 95% confidence intervals (CI) were estimated using Poisson regression.
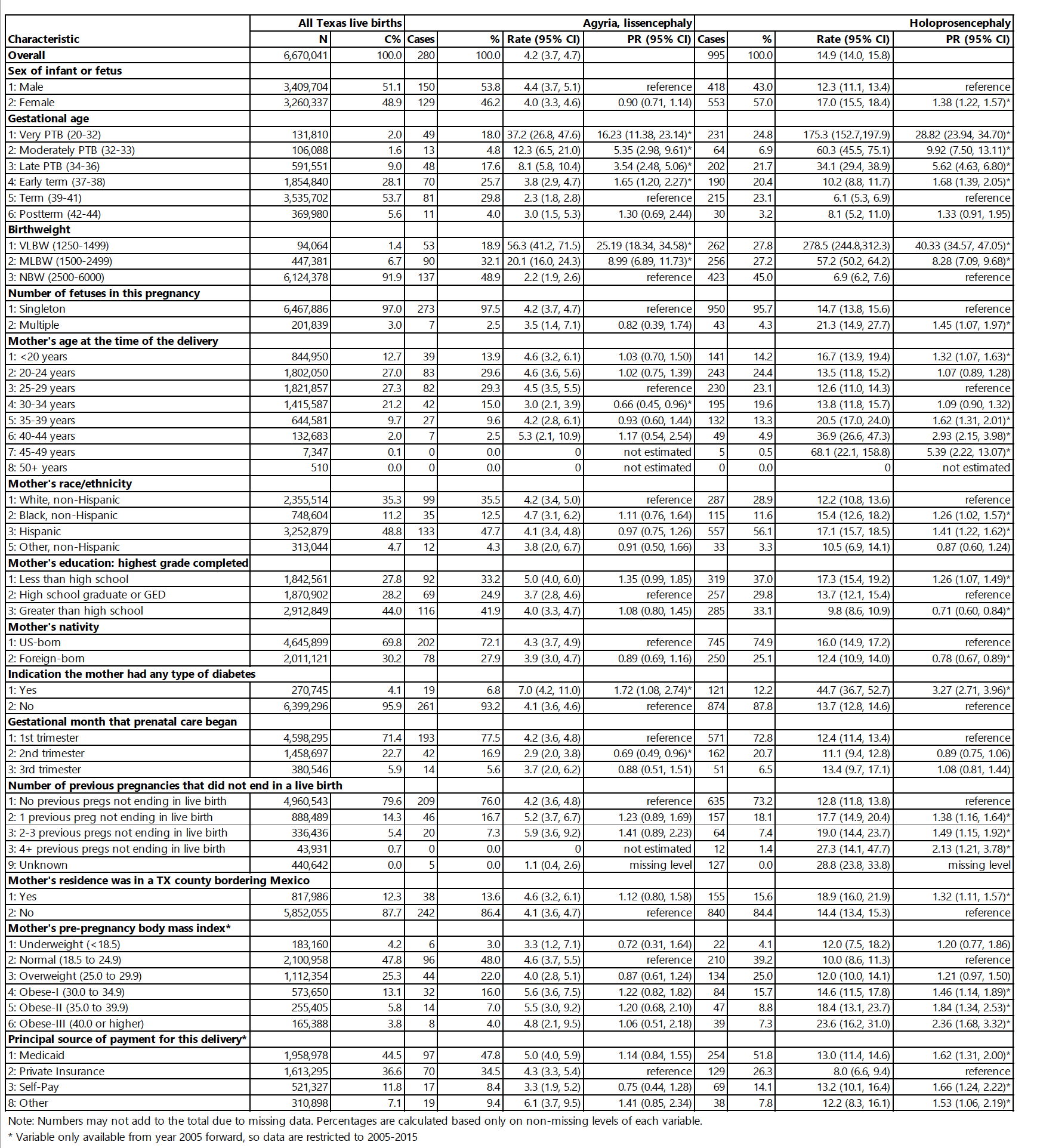
Results: Of 6,670,041 Texas live births during the study period, we identified 280 cases with LS for a rate of 4.2 per 100,000 live births and 995 with HPC, rate of 14.9 per 100,000 live births. The highest rates of LS and HPC were among cases delivered at < 32 weeks’ gestation and < 1500 grams. Maternal age < 20 years and > 35 years were significantly associated with increased likelihood of HPC diagnosis, as were maternal identification as non-Hispanic Black, and Hispanic, maternal diabetes, prior pregnancies not resulting in a live birth, Medicaid utilization, and living in a county bordering Mexico (Table 1). We also observed considerable geographic variability in prevalence of HPC and LS across the 11 Texas Public Health Regions (Figure 1).
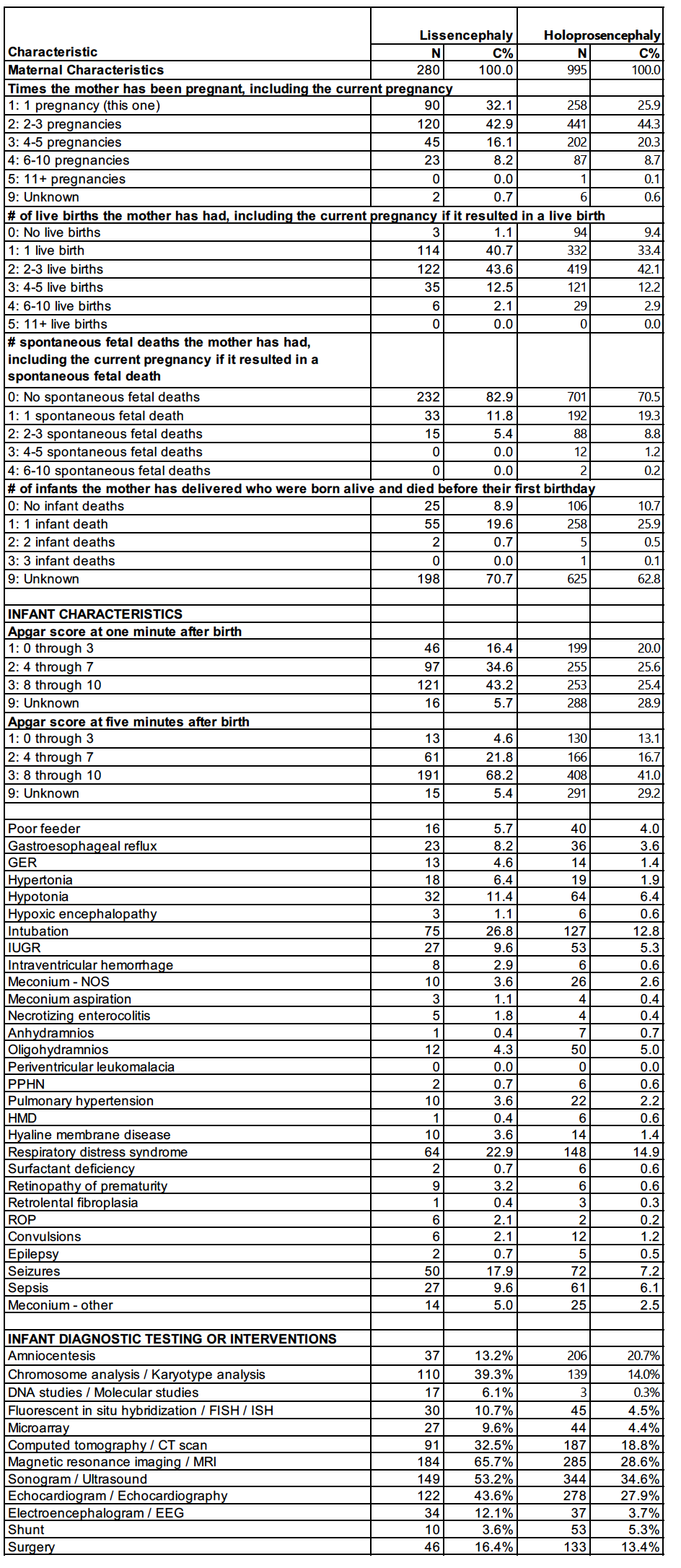
Infants with HPC had median Apgar scores of 6.0 and 8.0 at 1 and 5 minutes, respectively, whereas infants with LS had median Apgar scores of 7.0 and 8.0 (Table 2). The most frequently obtained diagnostic tests included MRI, CT scan, ultrasound, and echocardiography (Table 2). Common clinical findings included hypotonia, hypertonia, gastroesophageal reflux, and seizures.
Conclusion(s): We found several epidemiological and clinical characteristics associated with the diagnosis of LS and HPC. These infants are often sick at birth and require multiple diagnostic tests. Further investigation is needed into the factors associated with major CNS birth defects.