Neonatology
Session: Neonatal Neurology 4: Clinical
531 - The Effects of a Multimodal Environmental Modulation on Sleep Stage Distribution in Preterm Infants: A Randomized Controlled Trial
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 531
Publication Number: 531.1416
Publication Number: 531.1416
.jpg)
Toni P. Iurcotta, MD (she/her/hers)
Clinical Fellow
NewYork-Presbyterian Morgan Stanley Children's Hospital, Columbia University Medical Center
New York, New York, United States
Presenting Author(s)
Background: The neonatal intensive care unit (NICU) environment is a source of both sensory deprivation and developmentally inappropriate sensory stimulation that is disruptive to sleep-wake behavior development in preterm neonates. Sleep interventions to mitigate these harmful environmental effects on neurodevelopment are urgently needed.
Objective: To evaluate if a multimodal bassinet that mimics the intrauterine environment would provide more appropriate sensory stimulation and matured sleep state architecture with an increase in the percent total sleep time (TST) and quiet sleep (QS) duration.
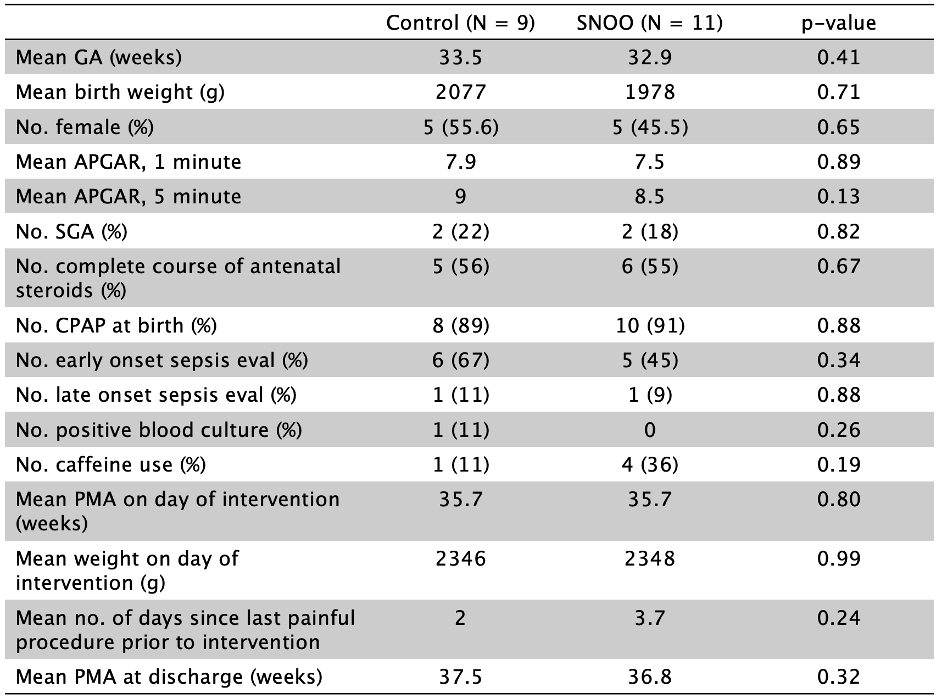
Design/Methods: A prospective randomized controlled study was performed in 20 preterm infants born between 28-36 weeks postmenstrual age (PMA) and admitted to a level IV NICU. The SNOO Smart Sleeper (SNOO), a multimodal bassinet that recreates features of the intrauterine sensory experience by combining rocking, swaddling, and white noise was chosen as an acute sleep intervention. When infants reached 35-36 weeks PMA, weighed >1.8 kg, and were off respiratory support in open cribs, they were randomized to be placed in a SNOO with full functionality (n=11) or in a powered-off SNOO (n=9) for a single 2-33-hour interfeeding period of observation. Infants’ behavioral states (QS, active sleep (AS), indeterminate sleep (IS), awake, and cry) were continuously coded each minute using a validated scoring system. TST in QS and AS was used as a proxy for neuromaturation for comparing the SNOO and control groups using Student’s t-tests.
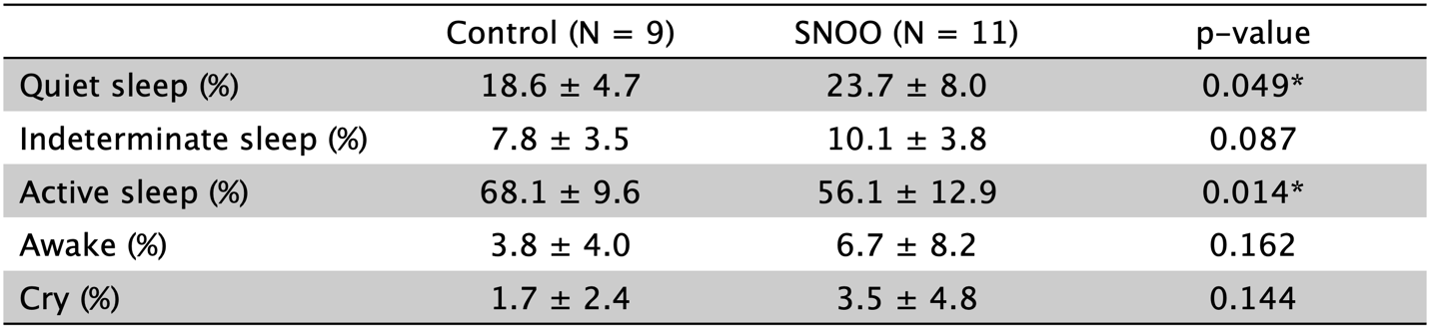
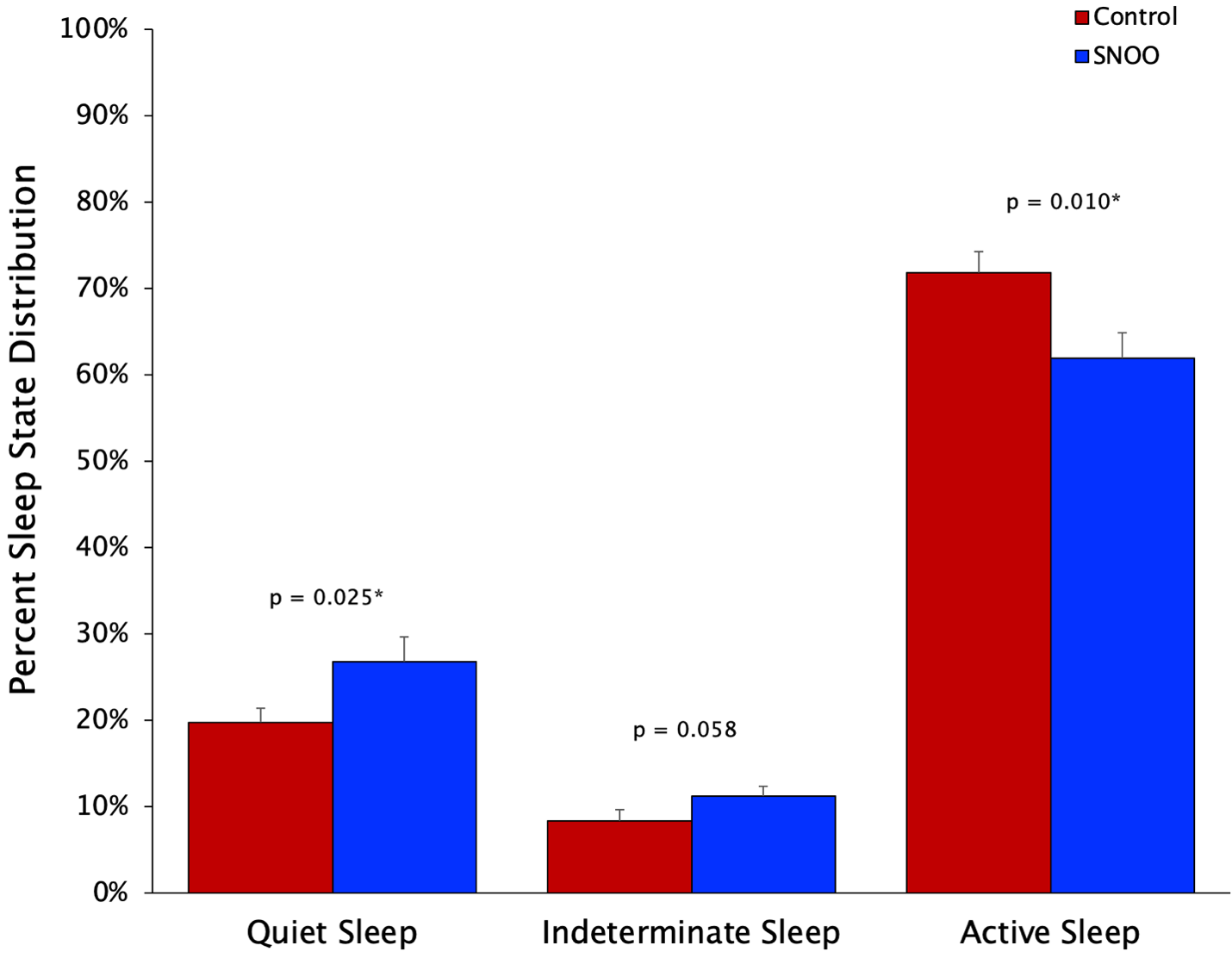
Results: The control and SNOO groups had similar characteristics (Table 1) with no difference in time spent asleep between the groups (89.9±12.3 vs. 94.5±5.5%, p=0.138). SNOO infants spent more time in QS (23.7±8.0 vs. 18.6±4.7%, p=0.049) and less time in AS (56.1±12.9 vs. 68.1± 9.6%, p=0.014) compared with the controls. There were no group differences in time spent in IS, awake, or crying (Table 2). When taking only TST into account, SNOO infants again spent more time in QS (26.8±9.5 vs. 19.8±5.1%, p=0.025) and less time in AS (61.9±9.8 vs. 71.8±7.5%, p=0.01) than controls (Figure 1).
Conclusion(s): Preterm infants exposed to SNOO multimodal sensory stimulation exhibited better sleep quality with higher %QS and lower %AS, both in the total study period and during TST. These data suggest that a brief exposure of preterm infants to multimodal vestibular, proprioceptive, and auditory modulation results in more mature sleep state architecture. Whether these effects on sleep-wake behavioral distribution persist and can influence long-term sleep health and neurodevelopmental outcomes needs to be evaluated.