Emergency Medicine
Session: Emergency Medicine 4: Infections
113 - Improving Antimicrobial Stewardship for Children with Skin and Soft Tissue Infections in the Emergency Department
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 113
Publication Number: 113.1317
Publication Number: 113.1317

Diane Kim, MD MPH (she/her/hers)
Emergency Department Pediatrician
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
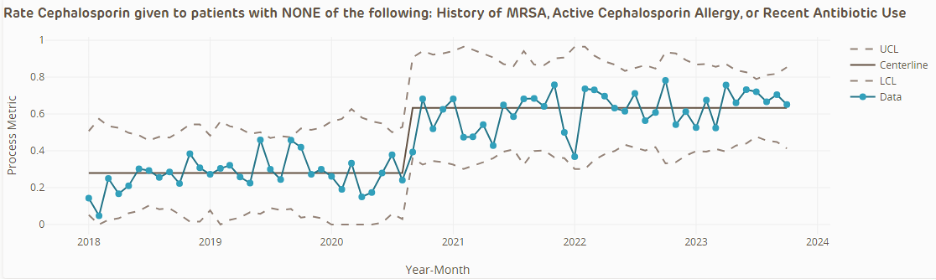
Background: In 2020, an increasing local prevalence of Methicillin Sensitive Staphylococcus Aureus (MSSA) compared to Methicillin Resistant Staphylococcus Aureus (MRSA) in Skin and Soft Tissue Infections (SSTI) was noted, as well as high rates of local clindamycin resistance in both MRSA and MSSA. The Children’s Hospital of Philadelphia modified its SSTI clinical pathway in September 2020 to switch the first line antibiotic recommendation from clindamycin to cephalexin (oral) or cefazolin (IV). This was thought to result in better overall empiric antibiotic coverage while decreasing the use of a broad spectrum antibiotic (clindamycin).
Objective: To improve antimicrobial stewardship for children with skin and soft tissue infections through clinical pathway revision (clindamycin to cephalexin/cefazolin as first line antibiotic choice) and clinical decision support. Balancing measures included 72 hour revisit and re-admission rates.
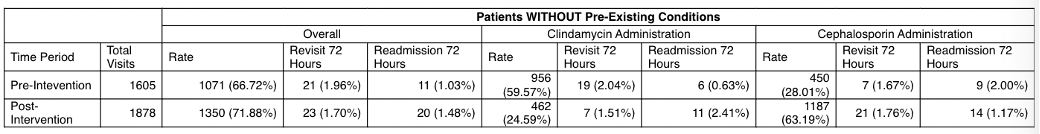
Design/Methods: A quality improvement initiative at a tertiary care, urban children’s hospital with over 100,000 annual Emergency Department (ED) visits. The hospital SSTI Pathway was edited September 2020 to change its first line antibiotic recommendation from clindamycin to cephalexin/cefazolin for those without MRSA risk factors or cephalosporin allergy. The Plan-Do-Study-Act (PDSA) cycle included Clinical Decision Support in the Electronic Health record to update both the ED and discharge order sets. In order to analyze compliance and balancing metrics, we compared treatment during January 2018-August 2020 (pre-pathway change) vs September 2020-October 2023 (post-pathway change). Subjects were patients 56 days to 21 years old with an ED visit for an ICD-10 code for cellulitis and abscess (ICD 10 blocks L02 and L03). Analysis included standard descriptive statistics.
Results: There were 1605 visits pre-pathway change and 1878 visits post pathway change. Rates of cephalexin prescription in children without risk factors for MRSA or cephalosporin allergy increased from 28% to 63% (p < 0.001) while rates of clindamycin prescription decreased from 60% to 25% (p < 0.001). There was no significant change in our balancing metric of 72 hour revisit rate (1.96% vs 1.70%, p=0.64) or re-admission rate (1.03% vs 1.48%, p=0.32).
Conclusion(s): There was improved antibiotic stewardship without a significant change in our balancing metrics of 72 hour revisit and re-admission rates for children with SSTIs. We were able to reduce the use of broad spectrum antibiotics based on changes in local antibiotic resistance patterns without a significant change in outcomes.
.png)
