Neonatology
Session: Neonatal Pulmonology - Clinical Science 1: BPD, BPD Biomarkers and Diagnosis
192 - Unsupervised learning from longitudinal ventilator settings and their association with BPD.
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 192
Publication Number: 192.2973
Publication Number: 192.2973
- MC
Milenka Cuevas Guaman, MD (she/her/hers)
Assistant professor
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Extremely premature infants (EPI) are at high risk for developing bronchopulmonary dysplasia (BPD). Early identification of EPI at risk of developing BPD can allow for targeted precision-medicine therapies. In this study, we sought to test the hypothesis that the longitudinal trajectories of early respiratory support can help identify EPI likely to develop BPD.
Objective: To use unsupervised machine learning to identify EPI clusters based on their longitudinal respiratory support and selected ventilatory settings trajectories and examine their association with clinical variables.
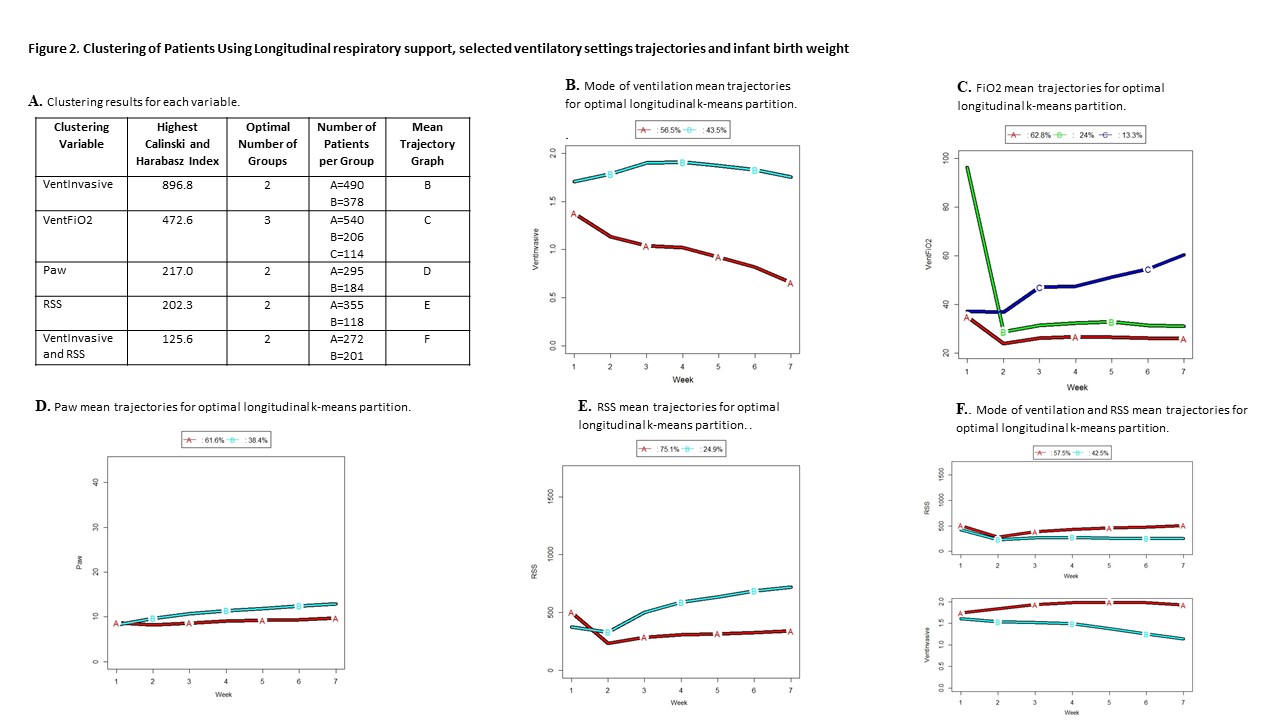
Design/Methods: We conducted a single-center, retrospective cohort review of the medical records of EPI admitted to a tertiary-care Level 3 NICU from January 2012 to December 2021. Data abstracted included demographics, maternal and birth data, and ventilator data weekly from birth for the first 6 weeks of life. The k-means algorithm for longitudinal variable trajectories was applied to identify patient clusters from longitudinal respiratory support and selected ventilatory settings. Cluster analysis was performed for the following variables:, invasive mechanical ventilation (VentInvasive), mean airway pressure (Paw), FiO2 and respiratory severity score (RSS= Paw *Fio2). Each variables’ trajectories over time were analyzed to partition the patients into groups. The partition with the highest Calinski and Harabasz (1974) index was used to select the optimal number of clusters. Associations of the groups were compared to clinical variables. The Kruskal-Wallis test was used to compare groups in terms of quantitative clinical variables whereas the Chi-square test was used for categorical clinical variables.
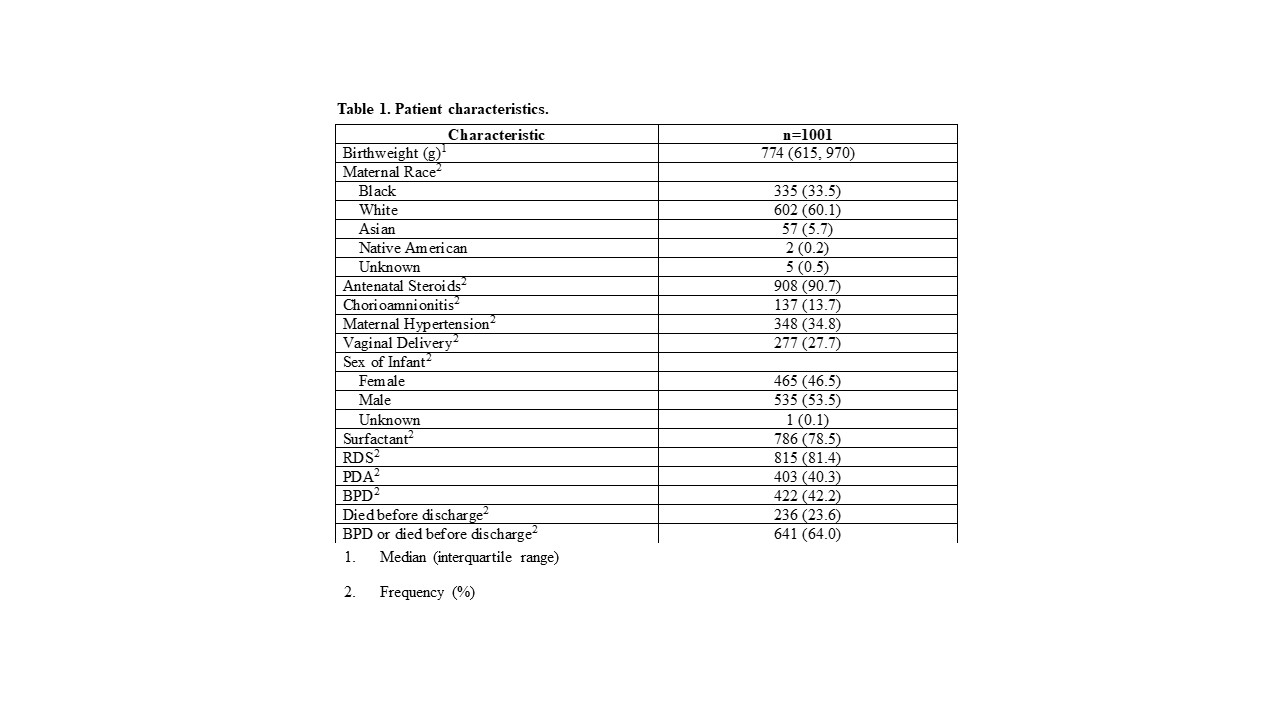
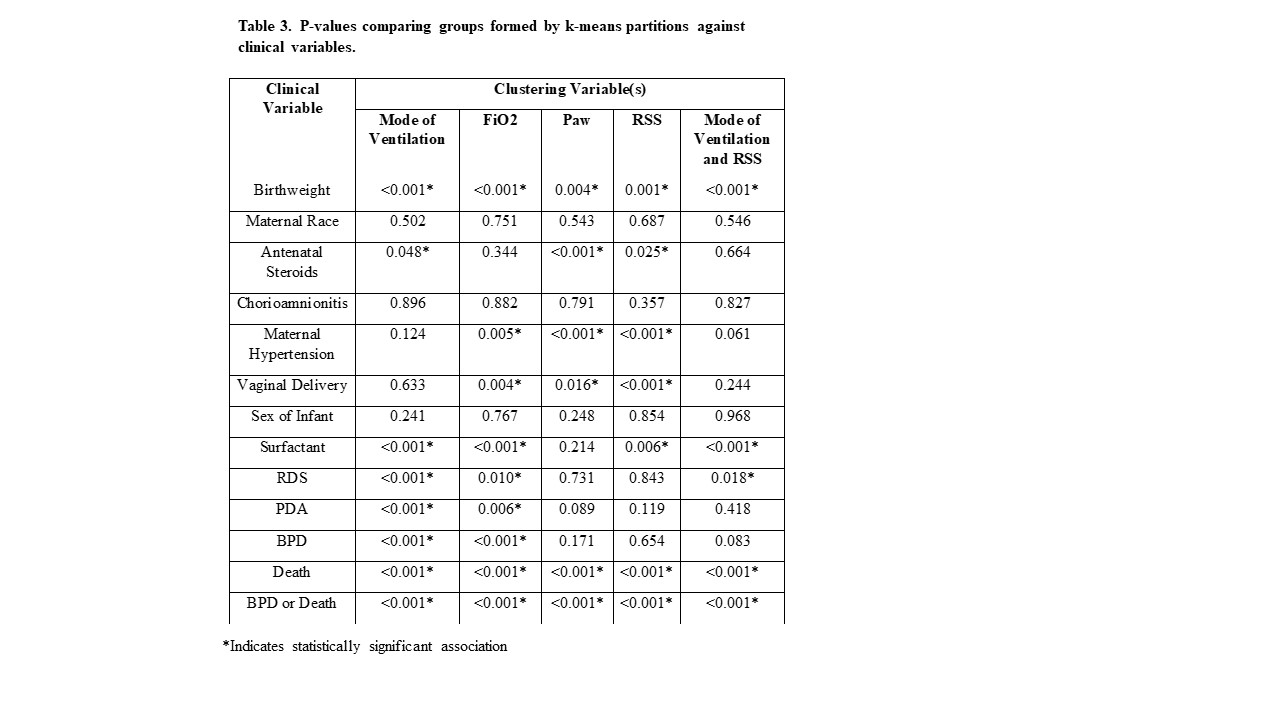
Results: Data from 1001 EPI with 6010 repeated ventilator observations were analyzed. Characteristics of the EPI are summarized in Table 1. The optimal number of groups and the number of EPI per group for each clustering variable are summarized in Figure 2A with longitudinal mean trajectories of clustering variables shown in Figure 2B-F. Table 3 demonstrates that EPI clusters from longitudinal respiratory support and ventilatory settings were significantly associated with important clinical variables including BPD and death.
Conclusion(s): Although previous research has applied unsupervised learning to mechanical ventilator data to classify patients with BPD, to our knowledge this is the first study to use unsupervised learning to classify EPI based on longitudinal trajectories of ventilator settings. The clusters were significantly associated with important clinical characteristics, including BPD.