Neonatology
Session: Neonatal/Infant Resuscitation 3
297 - Hospital Level of Service, Rural-Urban Hospital Location, and Neonatal Resuscitation Interventions at Birth: A Population-based Study in Alberta, Canada from 2000-2020
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 297
Publication Number: 297.2954
Publication Number: 297.2954

Breanna A. Pickett, MSc BSc (she/her/hers)
Student
University of Alberta
Edmonton, Alberta, Canada
Presenting Author(s)
Background: Advanced neonatal resuscitation interventions (ANRIs: endotracheal intubation, chest compressions, and epinephrine) are rarely needed for infants born at ≥34 weeks gestational age (GA). However, healthcare providers (HCPs) in community hospitals can encounter the need for ANRIs, while having less experience and resources than HCPs in centers with neonatal intensive care units (NICUs). Understanding practice differences between hospitals of different levels of service (LofS) and rural/urban location can inform quality improvement to reduce health disparities.
Objective: To examine how hospital level of service and rural/urban location relate to ANRI rates in Alberta, Canada, a universal public health system with standardized Neonatal Resuscitation Program (NRP) training.
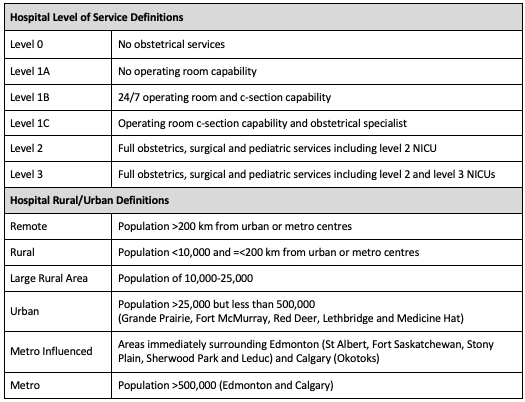
Design/Methods: All live births ≥34 weeks GA in Alberta from 2000-2020 inclusive were examined using retrospective, population-level administrative data from the Alberta Perinatal Health Program (APHP). Hospitals (n=97) were contacted to determine annual LofS during the study period, with levels (0,1A/B/C,2,3) based on provincial obstetrical triage for availability of delivery support, cesarean-sections, obstetricians, pediatricians/neonatologists, and NICUs. Hospitals were further subcategorized by population and proximity to metropolitan centers.(Table 1) Rates of individual interventions or any ANRI were compared.
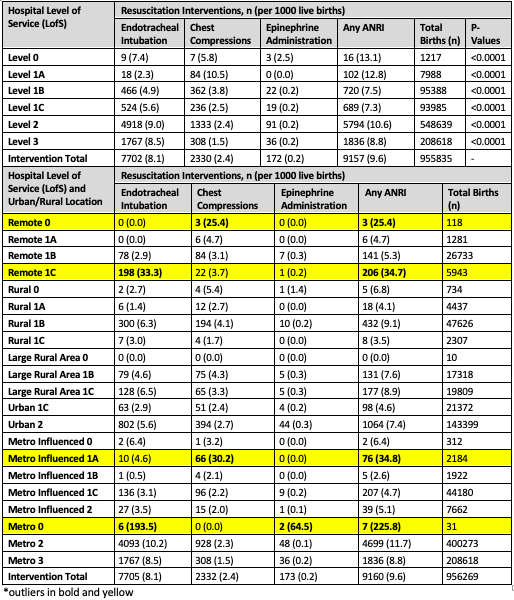
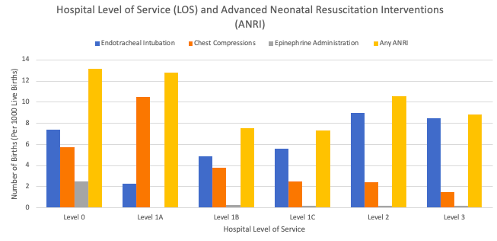
Results: There were 971,403 live births during the study period with a mean GA of 38.9 weeks; 1.6% were missing ANRI data, 955,835 births were included. Most occurred in hospitals with level 2 (57.4%) or level 3 (21.8%) NICUs; few occurred at sites with no delivery support (Level 0, 0.1%). ANRI rates were intubation (0.8%), chest compression (0.2%), and epinephrine (0.02%), any ANRI (0.96%, ~1/1000 live births). However, chest compression rates progressively decrease, and intubation rates progressively increase as LofS increases.(Table 2, Figure 1) When considering rural/urban location, there were outliers in chest compression rates in remote 0 (25.4/1000 live births) and metro-influenced 1A (30.2/1000 live births), intubation in remote 1C (33.3/1000 live births) and metro 0 (193.5/1000 live births) and epinephrine in metro 0 (64.5/1000 live births).
Conclusion(s): In this population-based cohort study of ≥34 weeks births, there were higher chest compressions rates and lower intubations rates at hospitals without NICUs despite standardized training. Reasons for this difference require further investigation; potential solutions such as targeted outreach education and introduction of laryngeal mask airways could be explored.