Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 1
363 - Lessons Learned from a National Multi-Center Trial on Pediatric Clinical Event Debriefing
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 363
Publication Number: 363.2082
Publication Number: 363.2082
Len Y. Tanaka, MD (he/him/his)
Assistant Professor
University of Hawaii, John A. Burns School of Medicine
Honolulu, Hawaii, United States
Presenting Author(s)
Background: Clinical event debriefing (CED) is a valuable tool for healthcare teams to identify strengths, weaknesses, and strategies to improve clinical practice and patient care. Developing local programs for CED can be challenging as time, space, personnel, and culture can affect both participation in and the utility of CED. The American Academy of Pediatrics (AAP) has created a program to provide resources and training to support institutions with different levels of experience in CED to successfully implement local programs. Identifying effective strategies and barriers for implementing CED will be important for creating an a national AAP CED program.
Objective: To identify the feasibility, facilitators, and challenges of implementing CEDs at pilot sites with different experience with conducting CEDs to guide for future expansion as a national program.
Design/Methods: AAP taskforce members with expertise in CED developed and iteratively revised the “Who, What, When, Where, Why and How in CED (WHiCED) Program” for pediatricians and pediatric subspecialists in 2020-22. Interprofessional teams from different institutions piloted the program as a Plan-Do-Study-Act (PDSA) cycle during 11/2022 to 2/2023. Teams completed a demographic survey and CED training. They conducted CEDs; tracked process, outcome, and balancing measures; and participated in a post-project focus group to discuss feasibility, facilitators, and challenges of implementing CEDs. Quantitative data were analyzed with descriptive statistics. Focus group transcripts were analyzed by thematic analysis.
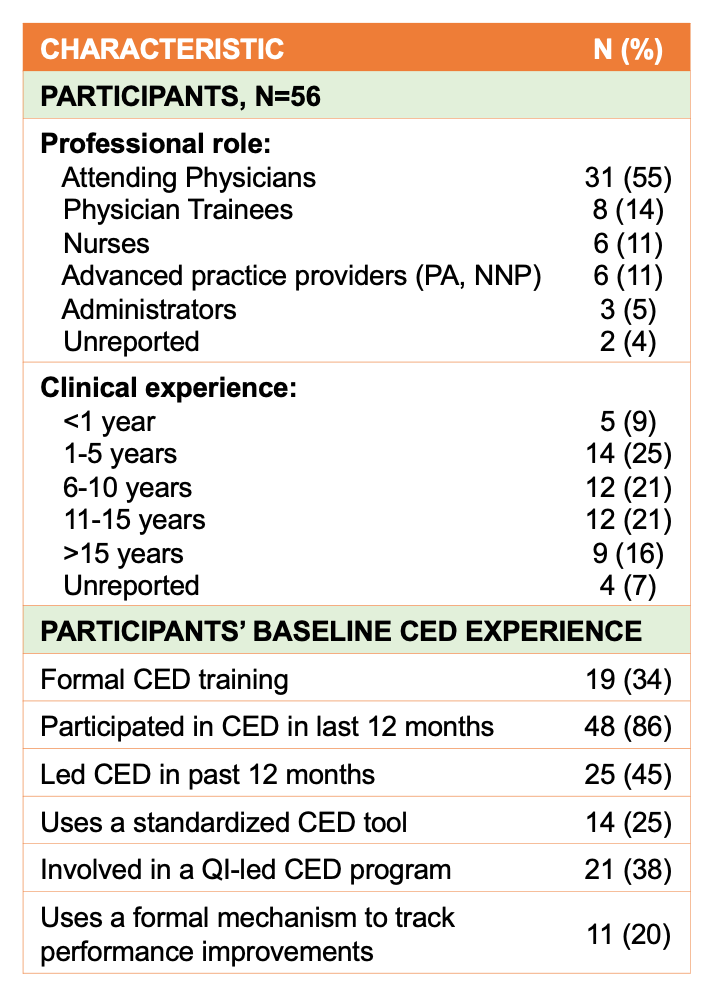
Results: Five teams (3 NICU, 1 pediatric ward, 1 PICU) from 4 sites participated, which included 56 participants with variable CED experience (Table 1). Among participants, 45% (25/56) never facilitated a CED. During the PDSA cycle, 58% (30/56) participated in 1-3 CEDs. The types and numbers of CEDs varied among sites (Table 2). In focus groups, sites identified strengths, weaknesses, opportunities, and threats to implementing the WHiCED program locally and nationally (Figure).
Conclusion(s): Pilot testing the WHiCED program built using a MOC Part 4 framework was feasible and was well-received by participants. Sites expressed successes and challenges in outcomes, process, and shared experiences, which highlight areas where the AAP may help support clinical settings with a wide range of CED resources and training to establish local CED programs across pediatric professions, disciplines, and practice settings.
.png)
.png)
