Immunizations/Delivery
Session: Immunizations/Delivery 1
42 - Parental Intent and Willingness to Vaccinate Children Under 5 against COVID-19 in the Pediatric Emergency Department
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 42
Publication Number: 42.1256
Publication Number: 42.1256

Harshini Sirvisetty, BA (she/her/hers)
Medical Student
University of Louisville School of Medicine
Louisville, Kentucky, United States
Presenting Author(s)
Background: While COVID-19 vaccine (CV) acceptance is improving, little is known about parental acceptance of CV in the pediatric emergency department (PED) or what interventions could improve uptake in this setting.
Objective: To determine rates of CV uptake among eligible children < 5 years old presenting to the PED, to compare parent willingness to accept CV in the PED over time, and to assess potential ED-based interventions to increase CV acceptance.
Design/Methods: In 2021, we conducted structured interviews with caregivers of children aged >= 6 months seen in a large, urban PED for minor illness/injury. Demographic data, COVID-19 and other vaccine history, and intent/willingness to receive future CV were recorded. Participants age < 5 years (n = 192) were re-contacted after vaccine eligibility to assess CV status, barriers to obtaining CV, willingness to obtain CV in the ED, and preferences for ED-based vaccine interventions (10-point Likert scale, 1 = not likely to persuade, 10 = most likely to persuade to vaccinate). Data were analyzed using standard descriptive statistics.
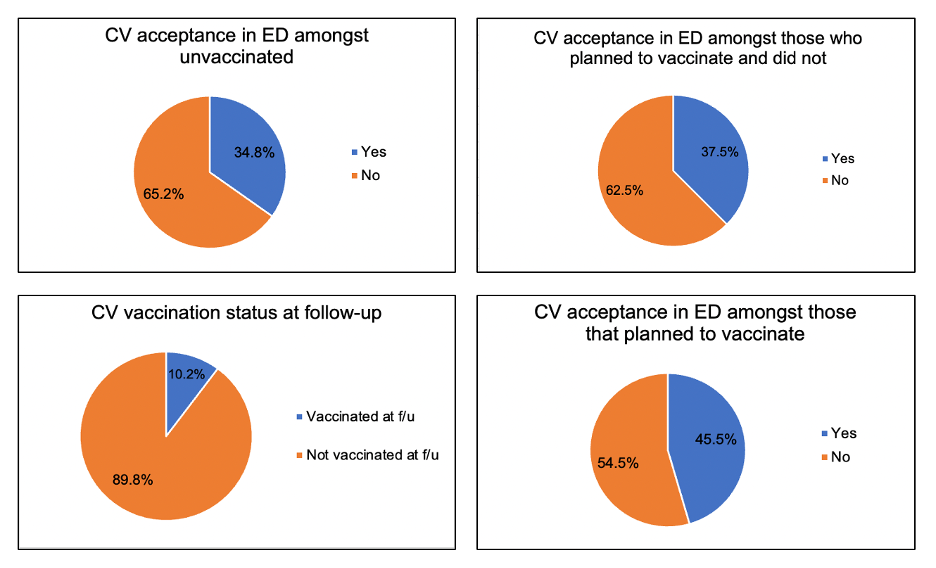
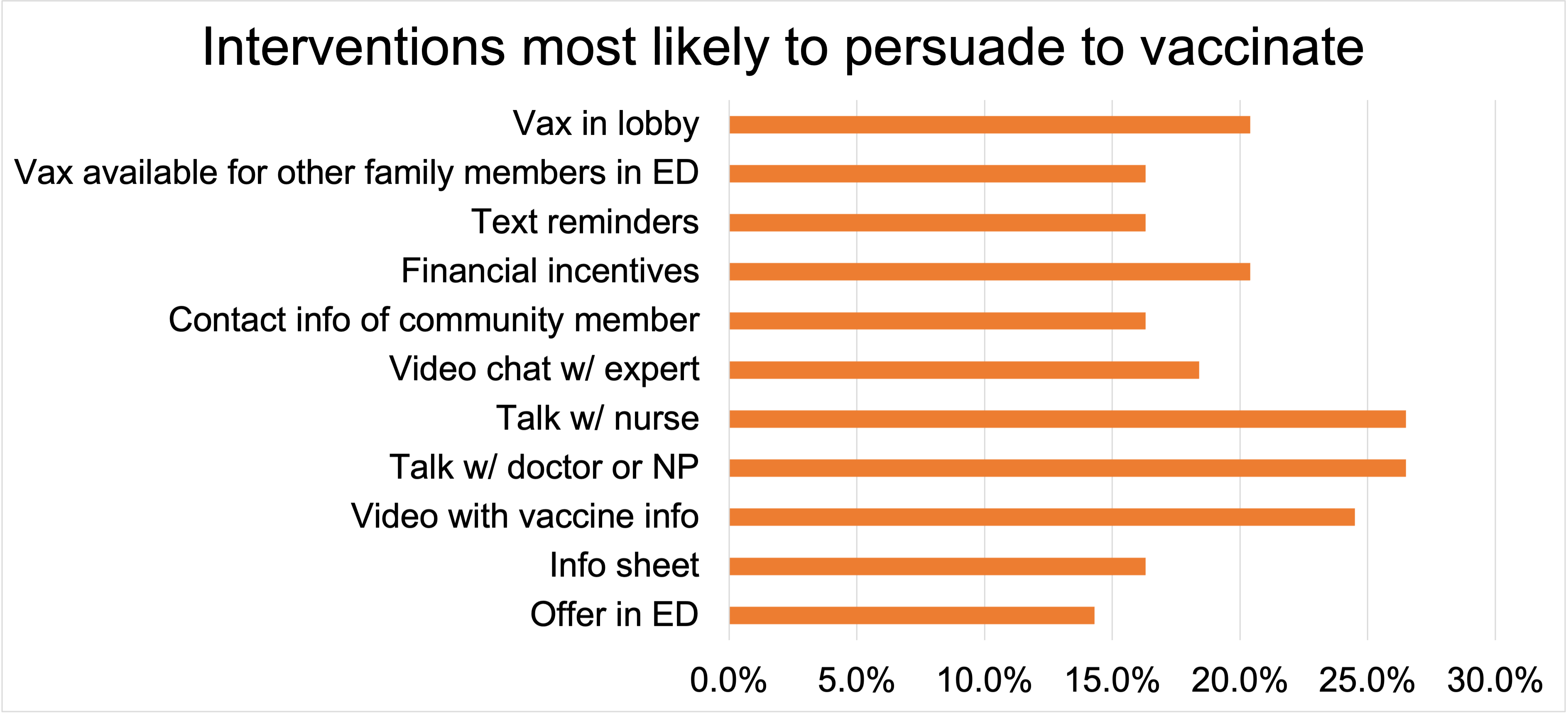
Results: Of 192 children < 5 from the original study, 141 (89.8%) were unvaccinated and 167 (87.0%) were reached in follow-up: 62 by phone and 105 by state immunization record review. Among unvaccinated children, 49 (34.8%) caregivers originally intended to vaccinate; 37.5% of those would accept CV in the ED. Of participants reached in follow-up; 17 (10.2%) had received CV. Among unvaccinated participants at follow-up, 11 (23.4%) originally planned to vaccinate; 5 (45.5%) would accept CV in the ED (Fig 1). Vaccinated families reported few barriers to access, most commonly lack of an easy time or place to obtain CV (10.7%). However, 1/3 of families whose children were unvaccinated at follow-up reported encountering barriers (most commonly, not knowing where to go/whom to call, 24.4%). Interventions most likely to persuade families to vaccinate (Likert scores 8-10/10) included: speaking with a provider about CV (26.5%), viewing a video with vaccine information (24.5%), or having vaccines available in the lobby/without an ED visit (20.4%) (Fig 2).
Conclusion(s): COVID-19 vaccine acceptance was low in this cohort but improved slightly over time. Our findings support a CV program in the PED: many caregivers intending to vaccinate their children would accept CV in the ED, some who otherwise remained unvaccinated. Interventions that may improve uptake include providing vaccine information (written or via personal discussion) and providing vaccines without a required ED visit.