Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 2: BPD and prematurity
101 - Acute Histological Chorioamnionitis Increases the Risk of Bronchopulmonary Dysplasia-associated Pulmonary Hypertension
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 101
Publication Number: 101.2261
Publication Number: 101.2261

Viral Jain, MD
Asst Prof
University of Alabama School of Medicine
Birmingham, Alabama, United States
Presenting Author(s)
Background: Acute Histological Chorioamnionitis (HCA) is a common cause of preterm birth (50-80%) and increases the risk of BPD. However, the association between HCA and BPD-associated pulmonary hypertension (BPD-PH) remains controversial. There is no proven treatment for HCA or preventing its associated adverse outcomes such as BPD-PH.
Objective: To determine (i) if extremely preterm infants exposed to moderate to severe HCA are at a higher risk of BPD-PH and (ii) develop an animal model to better understand the mechanism of HCA-induced BPD-PH.
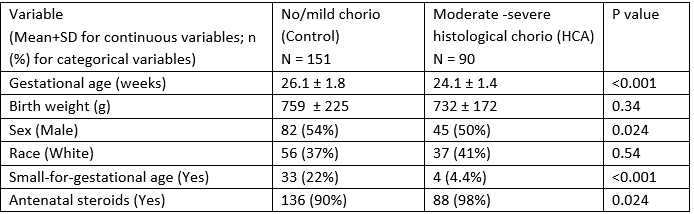
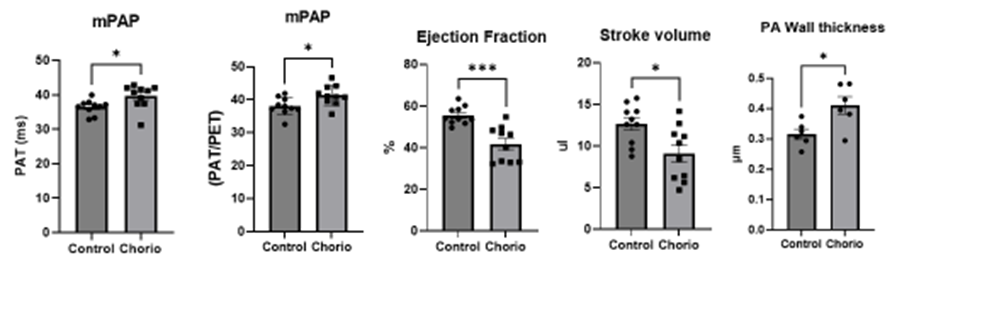
Design/Methods: This was a single-center retrospective cohort study of infants born between Jan 2017, and June 2021 at 22 0/7 to 28 6/7 weeks gestation who remained on respiratory support on postnatal day 28. Data from echocardiograms performed during the hospitalization after postnatal day 28 were included. Histological evaluation of placental pathology was graded into mild, moderate, and severe using standard criteria. A mouse model of chorioamnionitis was developed using pregnant dams at E16.5 injected with LPS in each amniotic sac (similar to human chorioamnionitis) followed by natural birth. BPD-PH in chorioamnionitis-exposed pups was assessed by pulmonary vessel wall thickness on histology and by Echo at 6 weeks. Pulmonary acceleration time (PAT) and the ratio of PAT/pulmonary ejection time (PET) assessed the mean pulmonary artery pressure (mPAP). Logistic regression was used to adjust for predefined variables.
Results: Of 241 infants, 90 (37%) were exposed to moderate-severe HCA while 151 had no/mild HCA (controls) (Table 1). Mod-severe HCA was associated with a higher risk of BPD-PH (OR: 1.88 [95% CI: 1.06, 3.34, p=0.030]) by multivariable analysis after adjusting for potential confounders (sex, antenatal steroids, small-for-gestation). In chorioamnionitis-exposed mice pups, an increase in mean pulmonary artery pressure as measured by PAT or PAT/PET was noted. A decrease in Stroke volume and Ejection Fraction suggestive of poor cardiac function was also seen. These mice also had an increase in pulmonary vessel wall thickness suggestive of pulmonary hypertension (Figure).
Conclusion(s): In extremely preterm infants, moderate-severe HCA increases the risk of BPD-PH. This increased risk of BPD-PH is also seen in a mouse model of chorioamnionitis. Further, ongoing studies are identifying mechanistic pathways involved in HCA-associated BPD-PH.