Breastfeeding/Human Milk
Session: Breastfeeding/Human Milk 2: Human Milk Feeding
490 - Mother's Own Milk at DOL 14 is associated with Breast milk at discharge for VLBWI in a Voluntary State Collaborative: Our continued journey.
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 490
Publication Number: 490.2246
Publication Number: 490.2246
- PK
Padmani Karna, MD (she/her/hers)
Neonatologist
Michigan State University College of Human Medicine
LANSING, Michigan, United States
Presenting Author(s)
Background:
Background: For very low birthweight infants (VLBWI), there is strong evidence that exposure to mothers’ own milk (MOM) feedings during the NICU hospitalization decreases the risk of potentially preventable complications of prematurity as well as their associated health care costs, including NEC, late onset sepsis, ROP, CLD and neurodevelopmental problems. This risk reduction is dose dependent. Neither donor human milk nor preterm formula provides comparable risk and cost reduction. Mothers of VLBWI are dependent on pumping for milk production, as their infants are not able to directly breastfeed until near the end of hospital stay. Previous research has shown that the first two weeks of pumping are critical to establish and maintain adequate milk production.
Objective:
Objectives: Our collaborative goal was to improve MOM at time of discharge for VLBWI in MI NICUs. We also assessed the relationship between % of feeds as MOM at 14 DOL with any MOM at discharge for VLBWI born 2018-2022.
Design/Methods: Methods: Voluntary Michigan NICU collaborative 15/18 NICUs have been promoting maternal breast milk (BM) feeding for VLBWI. All NICU teams were invited to 2 half day seminars to enhance BM provision. Driver Diagram was developed, challenges of breast pump quality and availability of lactation consultant were reviewed, and centers addressed best they could. Feeding guidelines were encouraged. Prospective data were collected in REDCAP. Infants who died, were transferred or were NPO at DOL 14 were excluded.
Results:
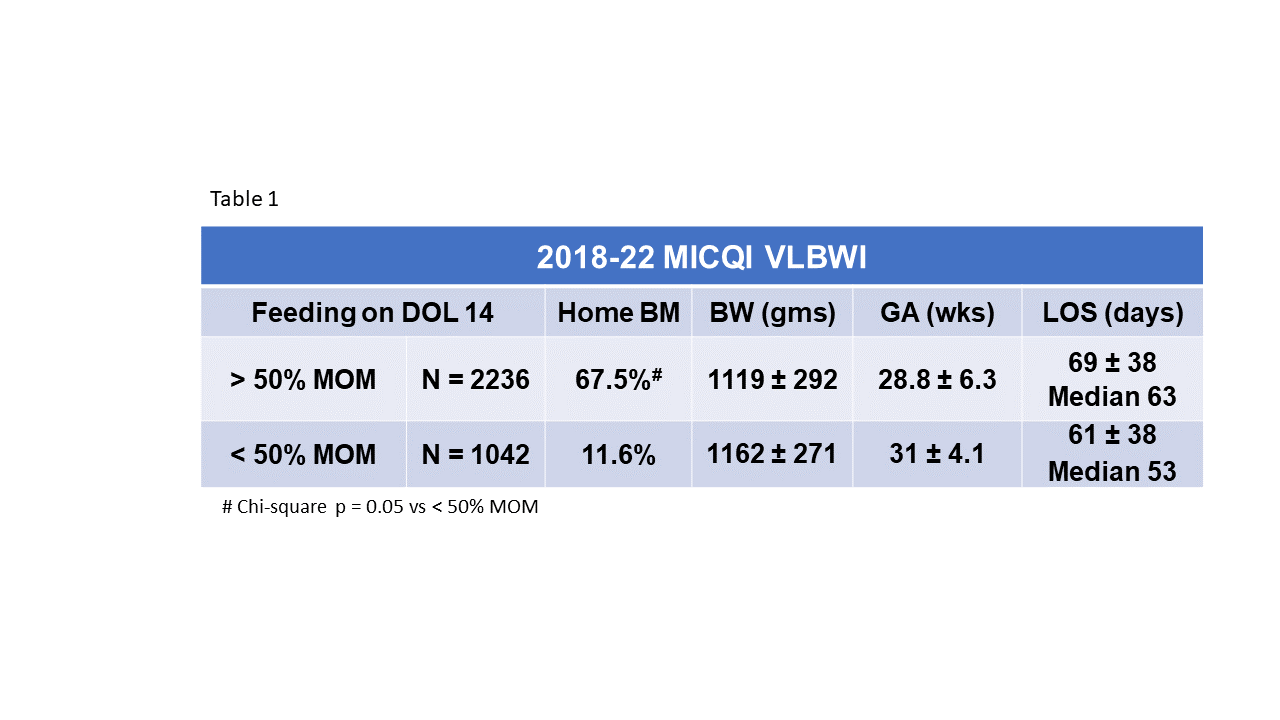
Results: In our state collaborative, MOM at discharge for VLBWI improved over time, from 42% in 2018 to 53% in 2022. Among VLBWI born 2018-2022 receiving >50% of feedings with MOM (with or without parenteral nutrition) on DOL 14, 68% were discharged with MOM versus only 12% for VLBWI receiving < 50% of feedings with MOM on DOL 14.
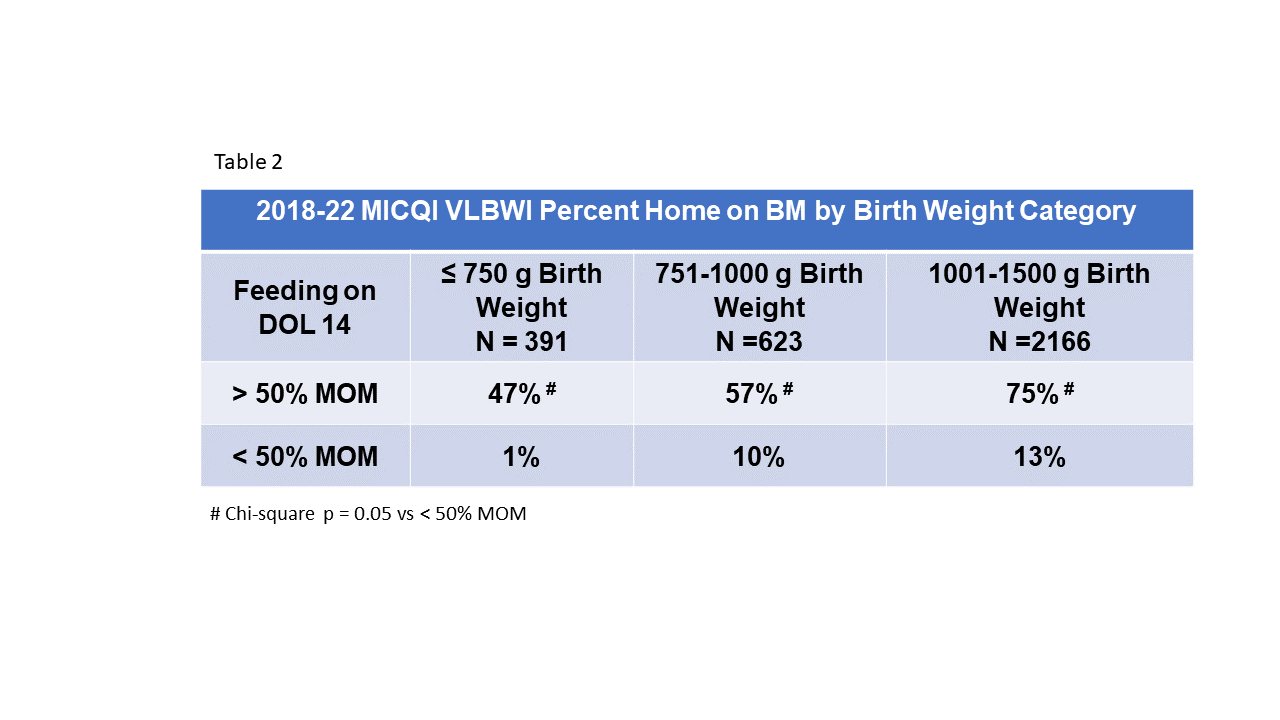
For infants BW < 750 grams who received >50% of feedings with MOM on DOL 14, 47% discharged with MOM vs 1% discharged with MOM if < 50% of feedings with MOM. For infants BW categories 751-1000 grams and 1001-1500 grams, there was a similar relationship with % MOM at 14 DOL but more of these infants discharged on MOM.
Conclusion(s):
Conclusions: In our voluntary state collaborative aiming to improve MOM at discharge, we found that >50% of feeds as MOM at DOL 14 is associated with ongoing MOM at the time of discharge for VLBWI. This relationship holds true regardless of BW category. Our data suggests that practices that support mother’s milk supply in the first 2 weeks of life help mothers continue to provide their own milk throughout the long hospital stay.