Neonatology
Session: Neonatal Pulmonology - Clinical Science 2: Lung Imaging, Lung Function
210 - Association between Lung Ultrasound Score and Large Patent Ductus Arteriosus (L-PDA) in Extremely Preterm Infants
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 210
Publication Number: 210.2796
Publication Number: 210.2796

Adel Mohamed, FRCPC (he/him/his)
Associate professor
University of Toronto Temerty Faculty of Medicine
Toronto, Ontario, Canada
Presenting Author(s)
Background: In preterm neonates with patent ductus arteriosus (PDA), surrogate echocardiographic features are usually employed for semi-quantitative delineation of shunt volume. Lung ultrasound score (LUS) has recently emerged as a non-invasive bedside tool for quantifying parenchymal disease severity; however, its utility in identifying preterm neonates with PDA is not known.
Objective: To examine the association between LUS and presence or absence of a large PDA (L-PDA, ≥ 1.5 mm) in preterm infants.
Design/Methods: Previously at our center 152 neonates born < 29 weeks’ gestational age (GA) had LUS documented within three days of birth for a prospective study, were considered eligible for inclusion. Among these, 54 who had also a clinical echocardiogram within 24 hours of LUS, documenting the presence of PDA, its diameter, and variables related to shunt volume (left ventricular output, left atrial to aortic root ratio). LUS was measured using a standard technique, assessing six regions in both lungs, with a total score ranging from 0 to 18. The neonates with a significant PDA (L-PDA) were compared to the rest of the cohort. Logistic regression was employed to explore the association between LUS and L-PDA, accounting for GA, antenatal steroid use, mechanical ventilation, and the respiratory severity score [RSS= fraction of inspired oxygen x Mean airway pressure) at the time of the scan. To evaluate linear correlations, Pearson's correlation coefficients were computed among LUS, RSS, PDA diameter, left ventricular output (LVO), and the left atrial to aortic root ratio (La:Ao).
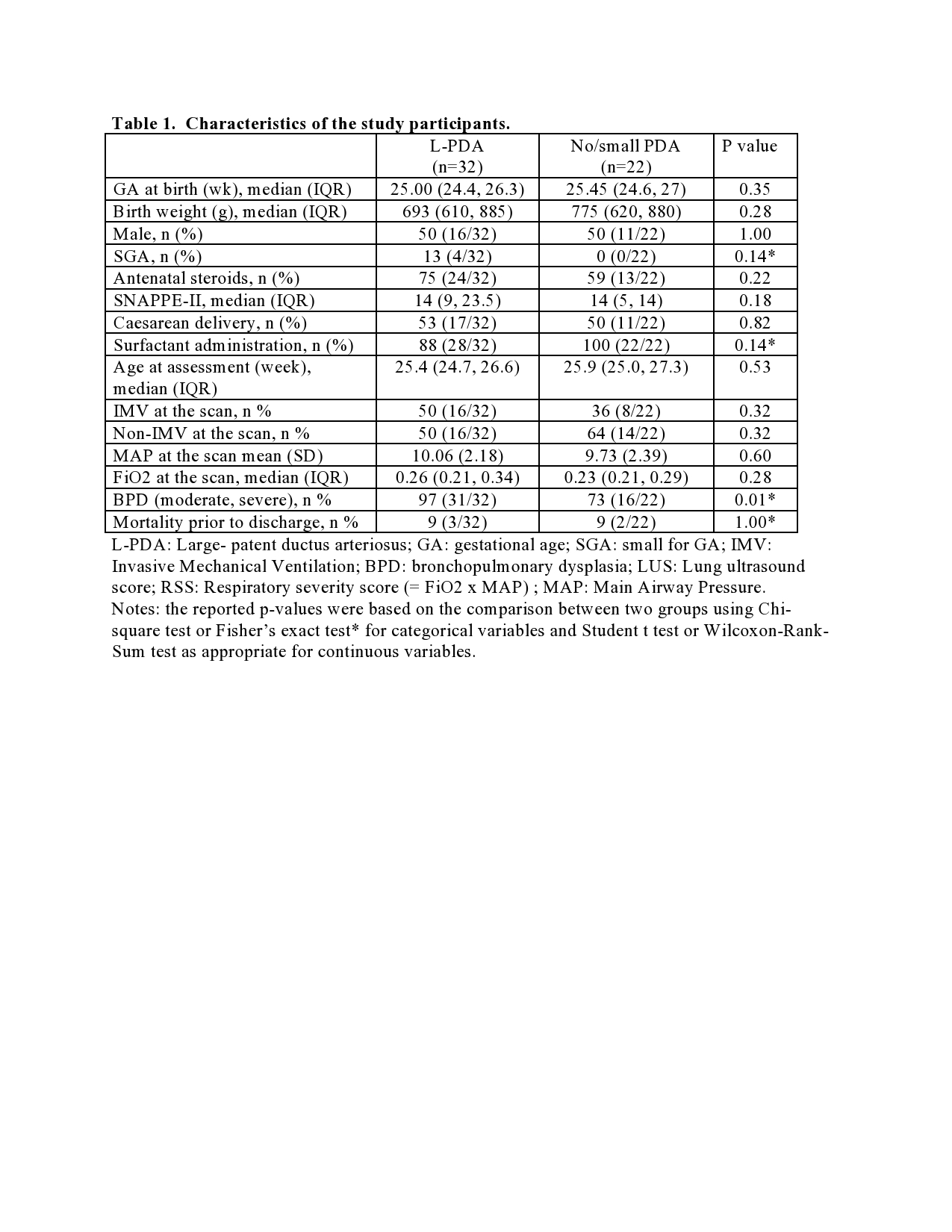
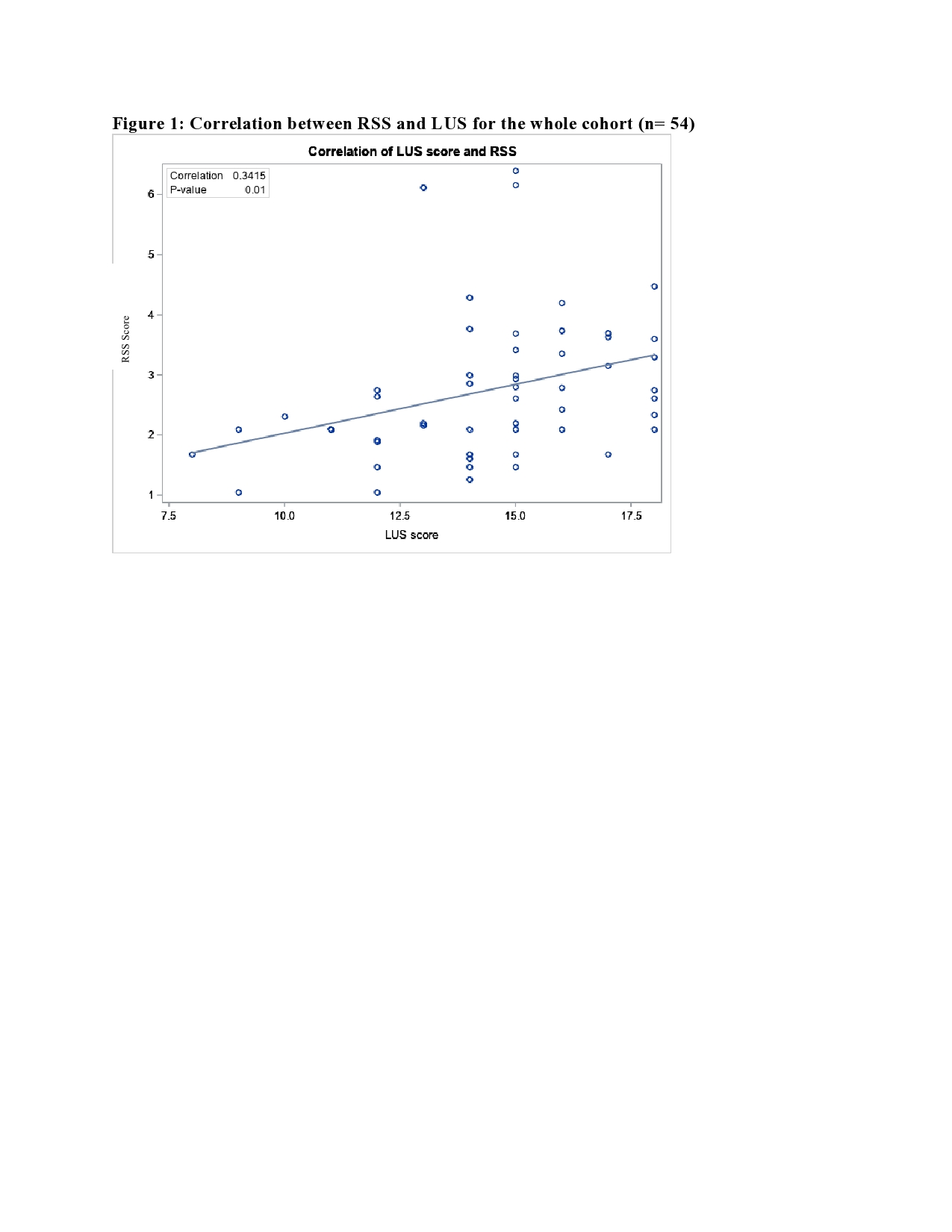
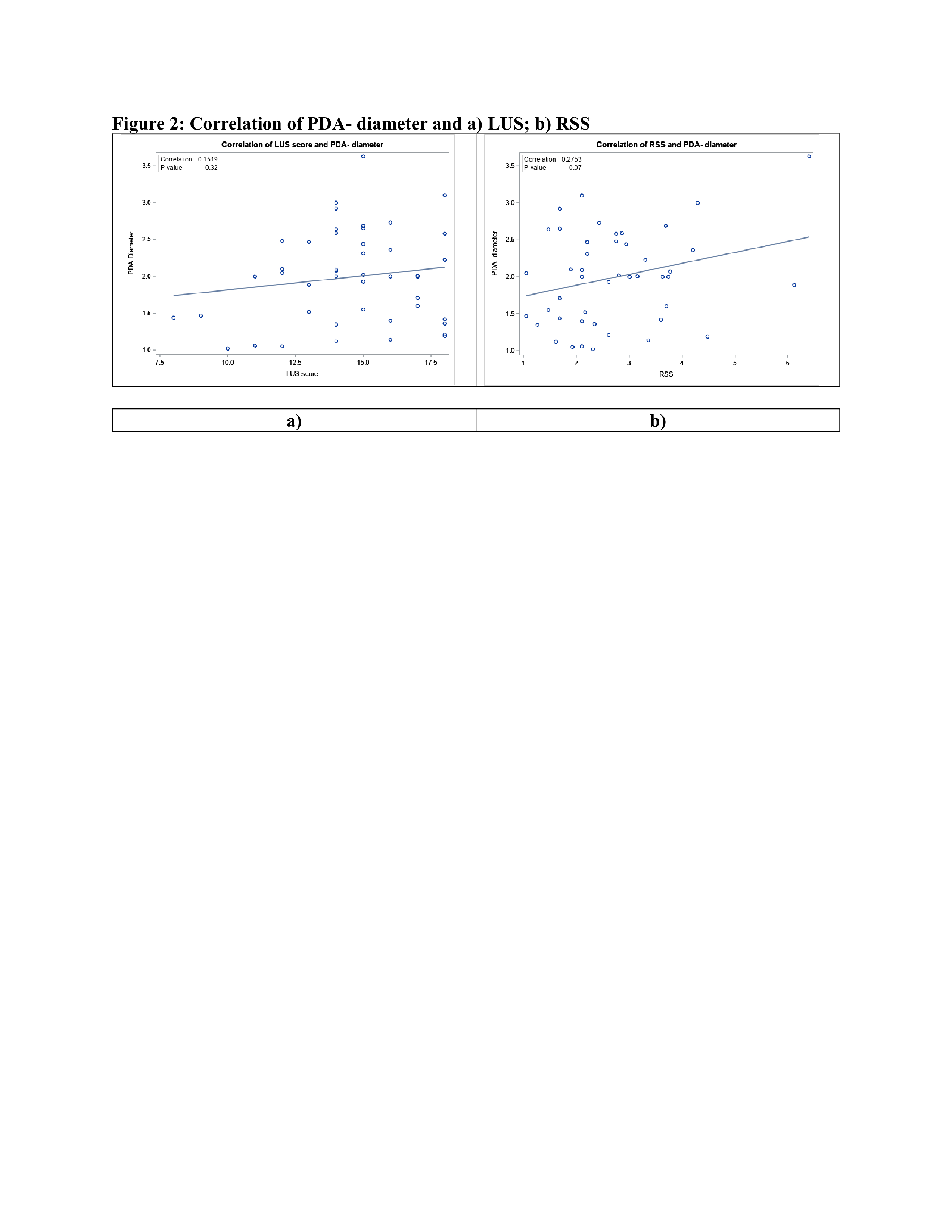
Results: Out of the 54 infants included, 32 (59%) had L-PDA. There was no difference in baseline characteristic between the two groups (Table 1). Both univariate and multivariate analyses revealed no significant difference in LUS between the groups (adjusted odds ratio 1.19; 95% CI, 0.89-1.59). Moderate-to-small positive correlations were seen between LUS and RSS, RSS and PDA diameter, but not between LUS and PDA diameter (Figure 1,2). No other significant linear correlation was seen between tested variables.
Conclusion(s): The lack of association between LUS and L-PDA during the first three days of life in this selected cohort of preterm infants may relate to the insensitivity of typical LUS to early signs of pulmonary over-circulation in the presence of evolving lung disease, or lack of contribution of L-PDA in pulmonary disease present during the time of assessments. Future studies should examine utility of LUS in PDA assessment beyond the transition period and longitudinally.