Neonatology
Session: Neonatal Pulmonology - Clinical Science 1: BPD, BPD Biomarkers and Diagnosis
193 - Early prediction of bronchopulmonary dysplasia by exhaled volatile organic compounds and glucocorticoid hormone levels in infants receiving non-invasive respiratory support: a feasibility study
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 193
Publication Number: 193.2816
Publication Number: 193.2816

Michelle Romijn (she/her/hers)
Research Fellow
Emma Children's Hospital Amsterdam UMC
Amsterdam, Noord-Holland, Netherlands
Presenting Author(s)
Background: Since respiratory management in preterm infants has shifted from primary invasive ventilation to non-invasive respiratory support, there is a need to early identify those non-intubated infants at high risk of developing BPD. Based on the hypothesis that an imbalance between inflammation and the anti-inflammatory hormone cortisol plays a key role in the multifactorial pathophysiology of BPD, we propose that adding glucocorticoid hormone levels to an existing BPD prediction model could have added value.
Objective: To investigate if a panel of glucocorticoid hormone levels (ie, cortisol, 17-OH progesterone, 11-deoxycortisol and cortisone) measured in blood and a combination of clinical predictors and volatile organic compounds (VOCs) in exhaled breath in preterm infants receiving non-invasive respiratory support in the first week of life increases the performance of that BPD prediction model.
Design/Methods: Infants born below a gestational age of 30 weeks without major congenital malformations were eligible for inclusion. At day 3 and day 7 of life, exhaled breath samples were collected to measure VOCs using gas chromatography-mass spectrometry, and blood samples to measure glucocorticoid hormone levels using liquid chromatography with tandem mass spectrometry. We added the glucocorticoid hormone levels to the National Institute of Child Health and Human Development (NICHD) clinical BPD prediction model and exhaled breath VOCs. From these models the predictive performances were calculated, including both discrimination and calibration, for the prediction of moderate to severe BPD.
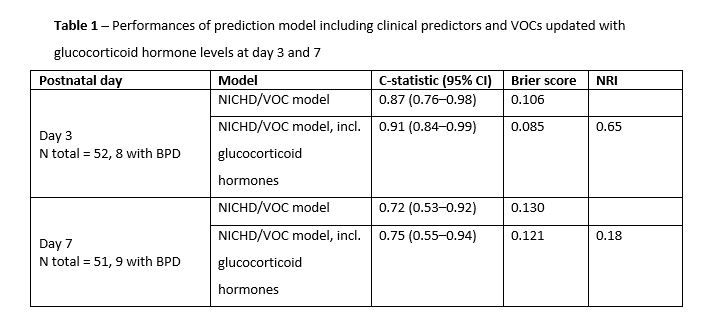
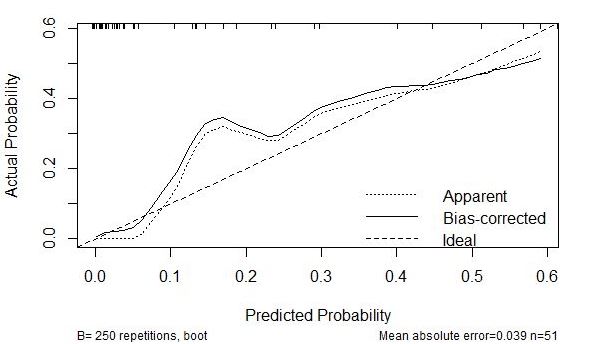
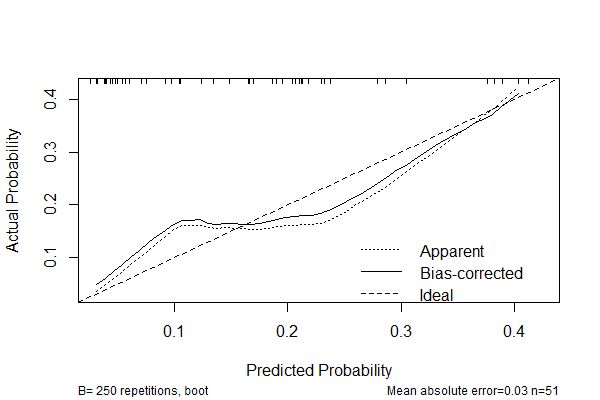
Results: In 58 infants both breath and blood samples were collected. Of these infants, 19% developed moderate to severe BPD at 36 weeks postmenstrual age. Addition of glucocorticoid hormone levels to the NICHD plus VOCs model at day 3 showed a c-statistic of 0.91 (95% confidence interval (CI) 0.84-0.99) compared with 0.87 (95% CI 0.76-0.98) without the glucocorticoid hormone levels. At day 7, the c-statistic of the updated model with glucocorticoid hormone levels showed 0.75 (95% CI 0.55-0.94), compared with 0.72 (0.53-0.92) without glucocorticoid hormone levels (Table 1). Calibration performances improved in the high predicted probability region at both days (Figure 1).
Conclusion(s): This study showed that addition of glucocorticoid hormone levels to a BPD prediction model based on clinical predictors and VOCs in exhaled breath might have the potential to improve the prediction of moderate to severe BPD in the first week of life in infants receiving non-invasive respiratory support.