Neonatology
Session: Neonatal/Infant Resuscitation 3
298 - The spectrum of endotracheal intubation practices among healthcare workers in newborn units in a low - and middle-income country.
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 298
Publication Number: 298.2853
Publication Number: 298.2853

Ikechukwu R. Okonkwo, MBBS FWACP MD (he/him/his)
Director of Neonatal Division
University of Benin Teaching Hospital
Benin City, Edo, Nigeria
Presenting Author(s)
Background: Advanced resuscitation (AR) is key to in-hospital newborn survival and neonatal tracheal intubation is one lifesaving skills for AR. It provides direct access to the lungs for ease of inflation during resuscitation and a stable interphase for sustained resuscitation and stabilization. It is also useful for surfactant replacement therapy (SRT) and mechanical ventilation (MV). This intervention is however not always available or possible in some newborn units in low- and middle-income countries (LMIC).
Objective: To assess intubation practices among Nigerian newborn care providers from different newborn units.
Design/Methods: A nationwide survey was done to assess newborn intubation practices among newborn care providers attending Paediatric Association of Nigeria (PAN) Conference 2022 & neonatal respiratory support workshops. The questionnaires were administered to willing and consenting attendees.
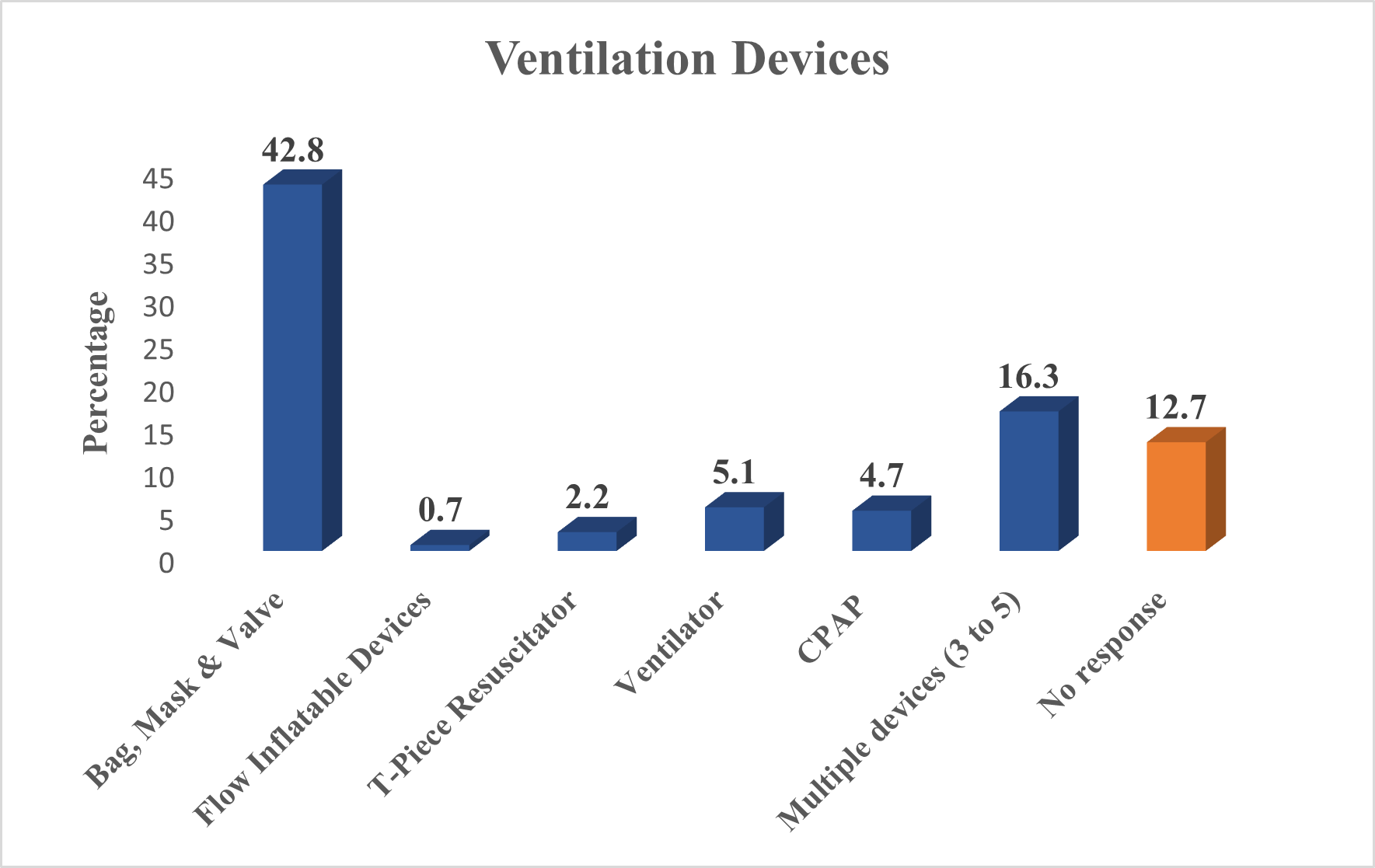
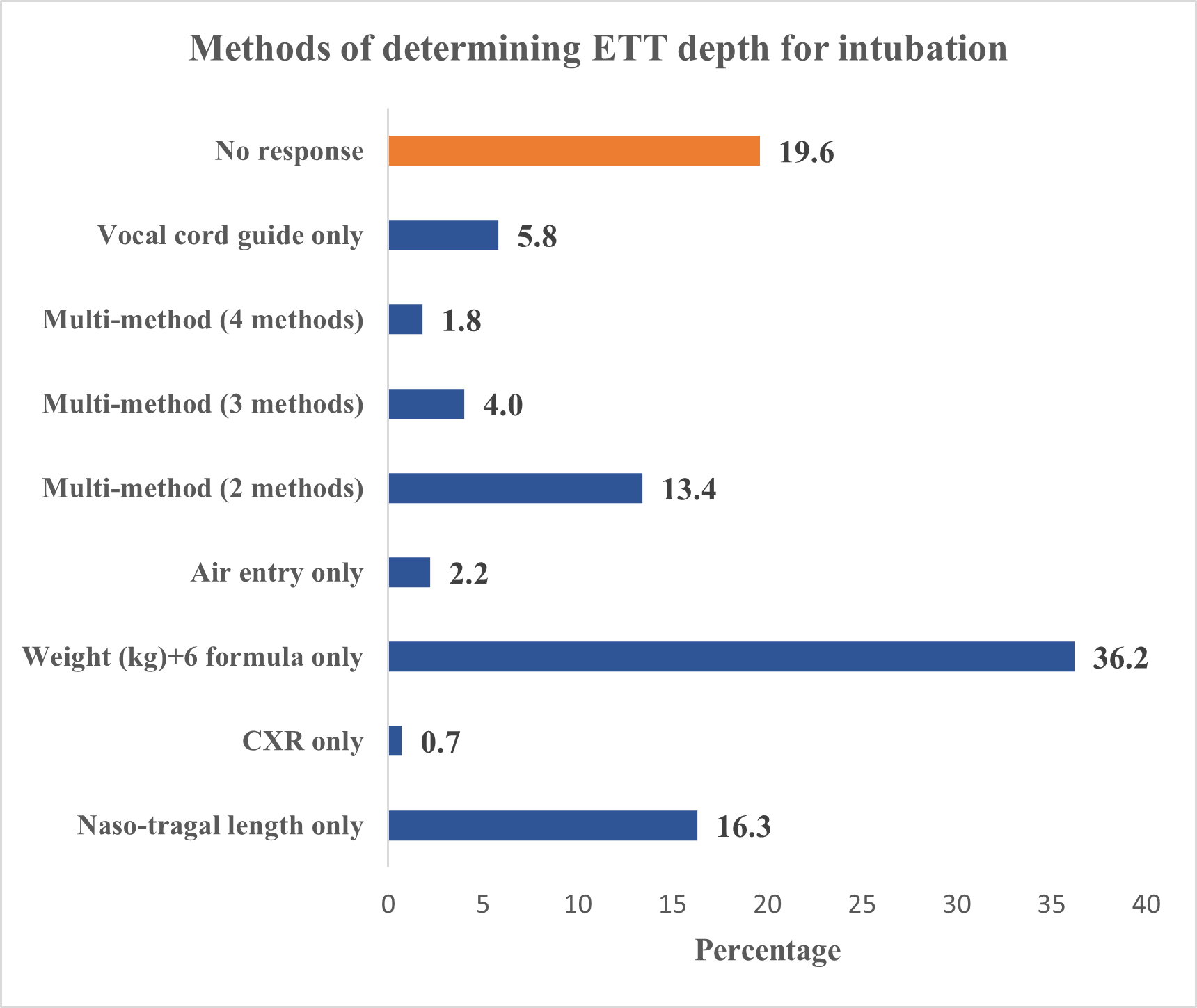
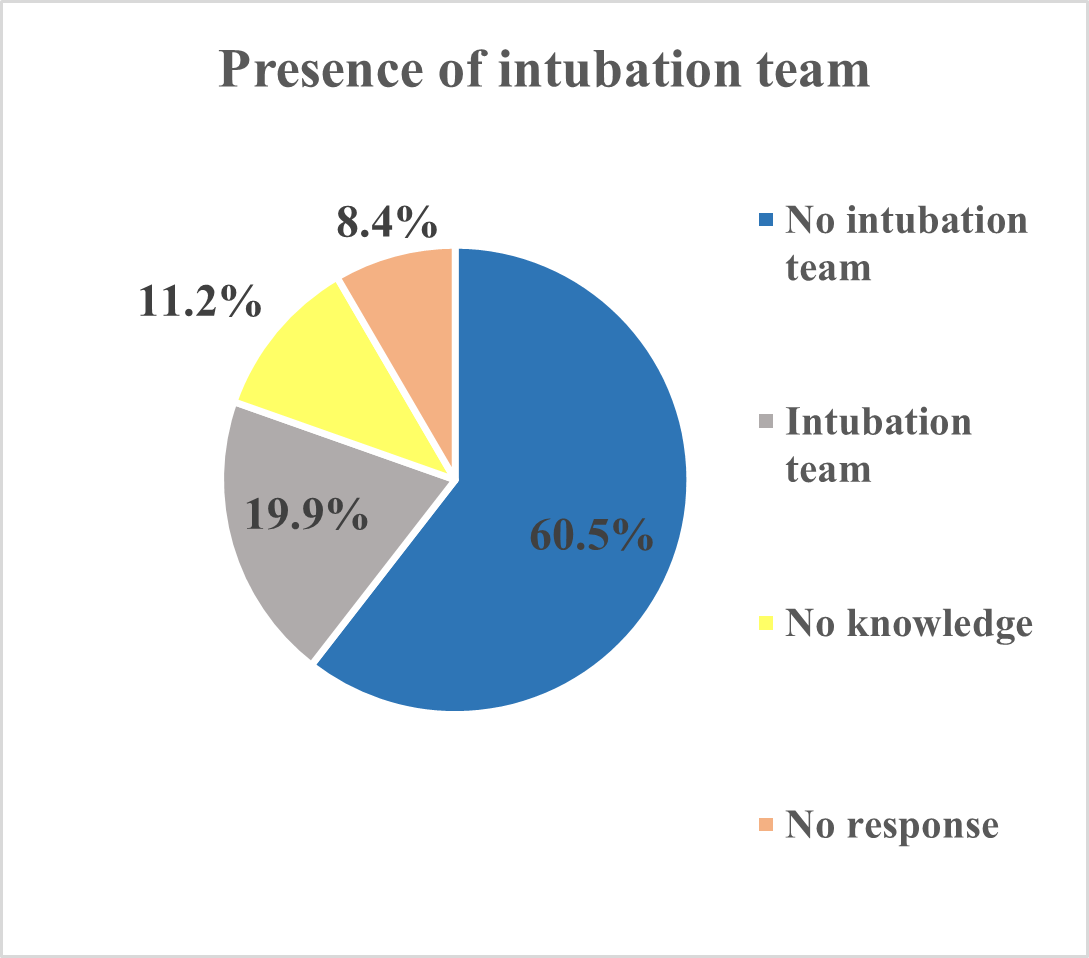
Results: A total of 300 questionnaires were distributed with 276 received back: a return rate of 92%. Most of the respondents were from public (85.9%) and tertiary (84.1%) care facilities. A combination of elective and emergency intubation was the most common (54%) followed by emergency (30.8%) intubation. Multiple indications (Resuscitation, SRT, MV, Surgery) were the commonest (22.5%) reason for intubation, followed by other indications (18.1%) apart from those already stated, resuscitation alone accounted for 14.1% of the reasons for intubation. SRT and MV accounted for equal proportion (6.5%) of indications for neonatal intubation. The Miller blade was the most common (34.4%) followed by Macintosh blade (15.9%). The number of laryngoscopes available in the unit were mostly one 72(26.1%) or two 76 (27.5%); the commonest blades were 00,0,1for 65 (23.6%) of the respondents. Disposable laryngoscopes were available to 28 (10.1%) of the respondents and unavailable to 223(80.8%). Intubated babies were mostly ventilated manually using BMV device by 118(42.8%) of the respondents. Neonatal intubations were performed by doctors 42 (14.5%). The formula Weight (Kg) + 6 was the most common (60.5%) means of determining endotracheal tube (ETT) depth of insertion; CXR was sparingly used for ETT depth of insertion. Intubation teams were only reported by 20% of the respondents.
Conclusion(s): AR is slowly evolving in some low- and middle-income countries like Nigeria. There is paucity of neonatal intubation resources, skills and capacity which is a determinant of enhanced survival of sick newborns. There is a need for training and task shifting to other cadres of staff to perform these lifesaving interventions.