Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 4: Congenital Heart Disease
178 - Predictors of Gastrostomy Tube Placement in Newborns with Major Congenital Heart Defects Undergoing Surgery
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 178
Publication Number: 178.2849
Publication Number: 178.2849

Angel Sunny, MD (she/her/hers)
Pediatric Resident
Mount Sinai - Elmhurst
Queens, New York, United States
Presenting Author(s)
Background: Feeding difficulties and the need for gastrostomy tube placement (GT) in newborns with congenital heart
defects (CHD) who undergo cardiac surgery are very common. Failure to achieve full oral feeding at discharge is
associated with neurodevelopmental delays and the identification of risk factors associated with this can help
to devise strategies that improve the outcomes for these infants. However, the few studies that have examined
these risk factors are single-center studies with small sample sizes and mixed results.
Objective: To identify the prevalence and the factors associated with GT placement at discharge in newborns with CHD
who underwent cardiac surgery during the birth hospitalization.
Design/Methods: This was a retrospective, cross-sectional analysis of the 2016 and 2019 Kids Inpatient Database. Newborns
(admission age < 28 days) with major CHD who had cardiac surgery (assigned a Risk Stratification for Congenital
Heart Surgery) were identified with ICD-10 codes, and those who survived to discharge were dichotomized into
those with and without GT. Infants with isolated cardiac defects (PDA, VSD, ASD) were excluded. The
demographic and perinatal characteristics, and the hospital course were compared using Chi-square or
Wilcoxon-Rank sum test, as appropriate. The exposure variable was CHD with cardiac surgery and the
outcomes of interest were the prevalence and predictors of GT placement. A priori set of covariates and other
clinically relevant variables were entered into a multivariable logistic regression analysis to identify the
predictors of GT placement.
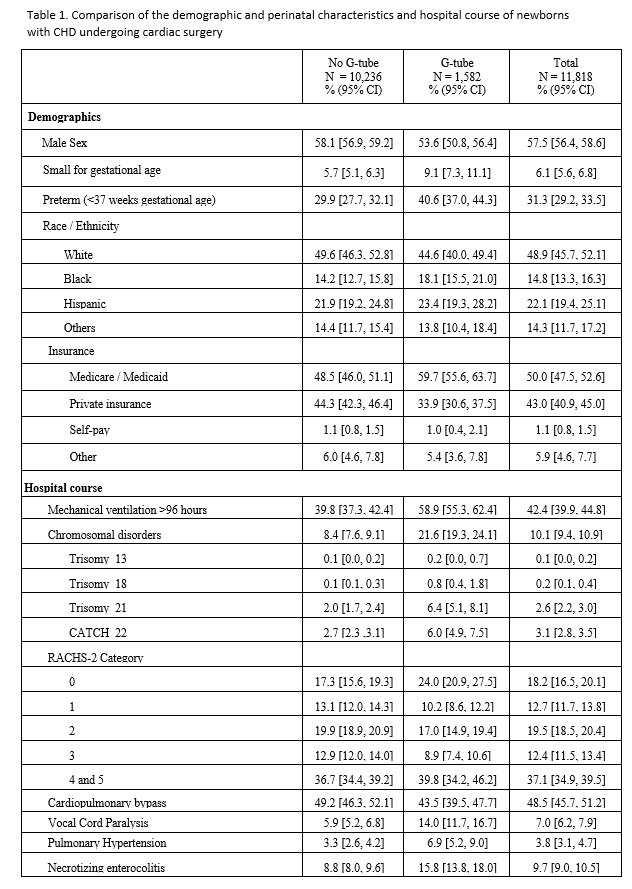
Results: Among 7.724 million neonatal admissions, 38,053 had CHD (4.9/1000). Of these, 11,818 had RACHS-2
classification and were included in the study. The prevalence of GT was 13.3% (1,582/11,818). The
characteristics of the study population are shown in Table 1. Compared to those without GT, those with GT
were more likely to have Medicaid, be ventilated for >96 hours, be preterm, have chromosomal disorders, have
vocal cord paralysis, pulmonary hypertension, and longer length of stay (89 vs 31 days) and higher hospital cost
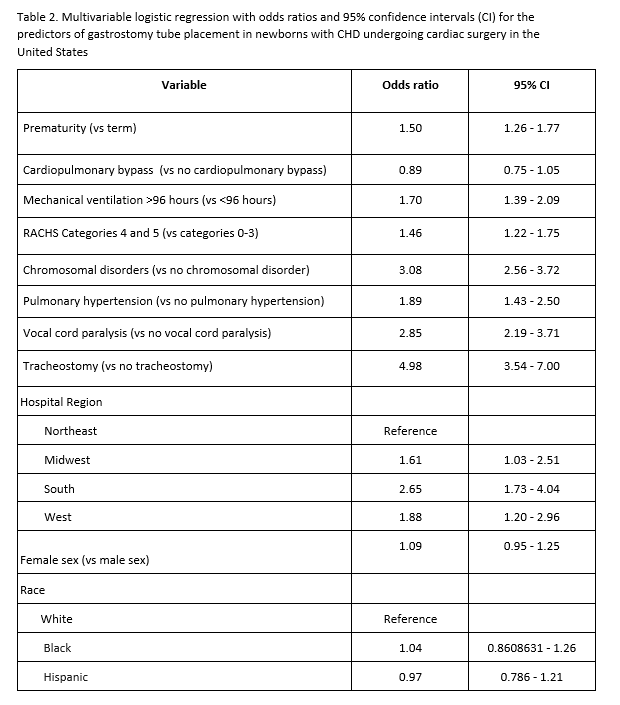
($349,479 vs 172,847). In the adjusted analysis (Table 2), tracheostomy placement, prematurity, mechanical
ventilation >96 hours, chromosomal disorders, pulmonary hypertension, RACHS-2 ≥4, and vocal cord paralysis.
Cardiopulmonary bypass and sex were not associated with increased odds of GT placement.
Conclusion(s): These findings can be used for counseling families and the early identification of newborns who would require
GT can potentially reduce length of stay and hospital cost.